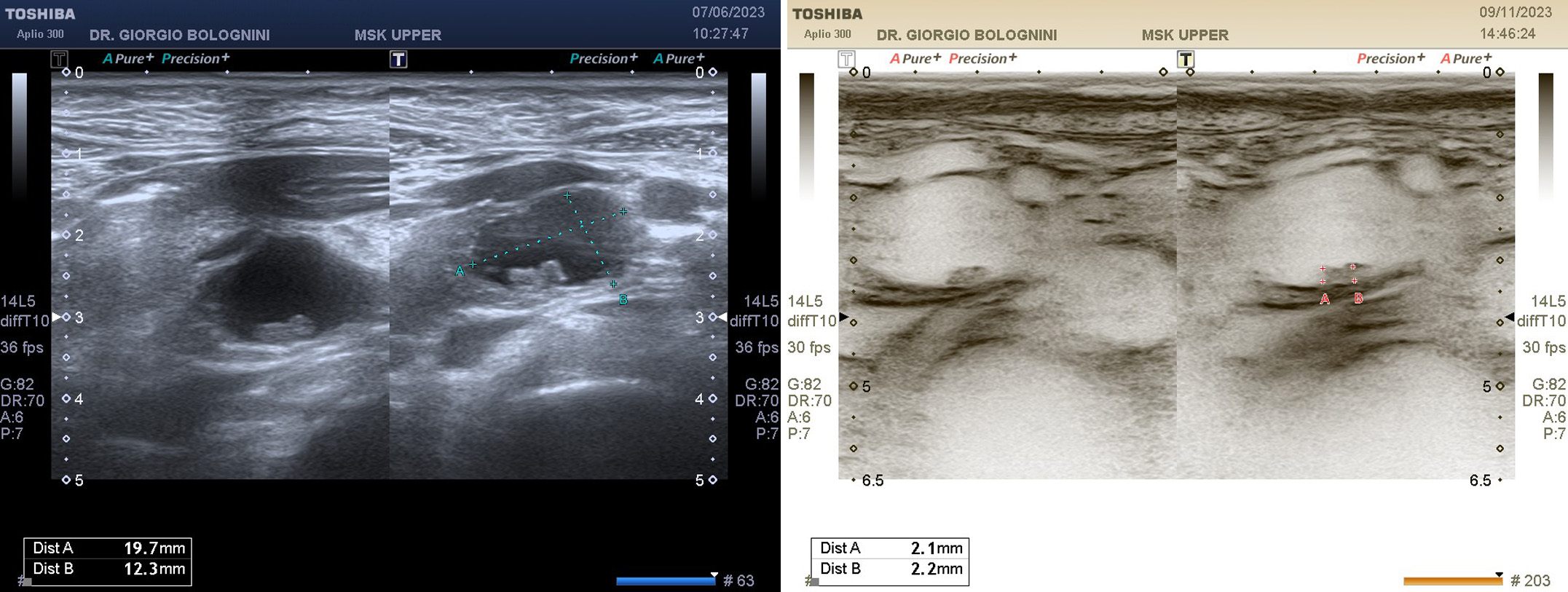
55-year-old woman, operated on for infiltrating lobular breast cancer with total mastectomy and currently undergoing suppressive hormone therapy; comes to my ultrasound clinic for abdominal oncological follow-up in addition to hospital checks. During the examination I detected the presence of an oval cystic formation in the pancreatic uncinal region of approximately 17.6x15.6mm, not reported in the previous instrumental tests, with some solid wall thickenings, the two largest on the posterior wall of approximately 2mm each, adjacent; echogenicity respected in all areas. Wirsung with a maximum caliber of 2mm with a non-tortuous linear progression. Regular portal system for caliber and flows. Presence of reactive lymph nodes at the level of the anterior pillar of the omental bursa, the largest with a long axis of approximately 8mm; other reactive lymph nodes are identified at the level of the pericecal mesentery in FID. Further presence of two hyperechoic nodular formations compatible with simple angiomas at the level of the VII hepatic segment of 11mm, and at the level of the III hepatic segment at the lower margin of approximately 13mm. I therefore recommend performing an abdominal MRI with contrast medium for diagnostic confirmation.
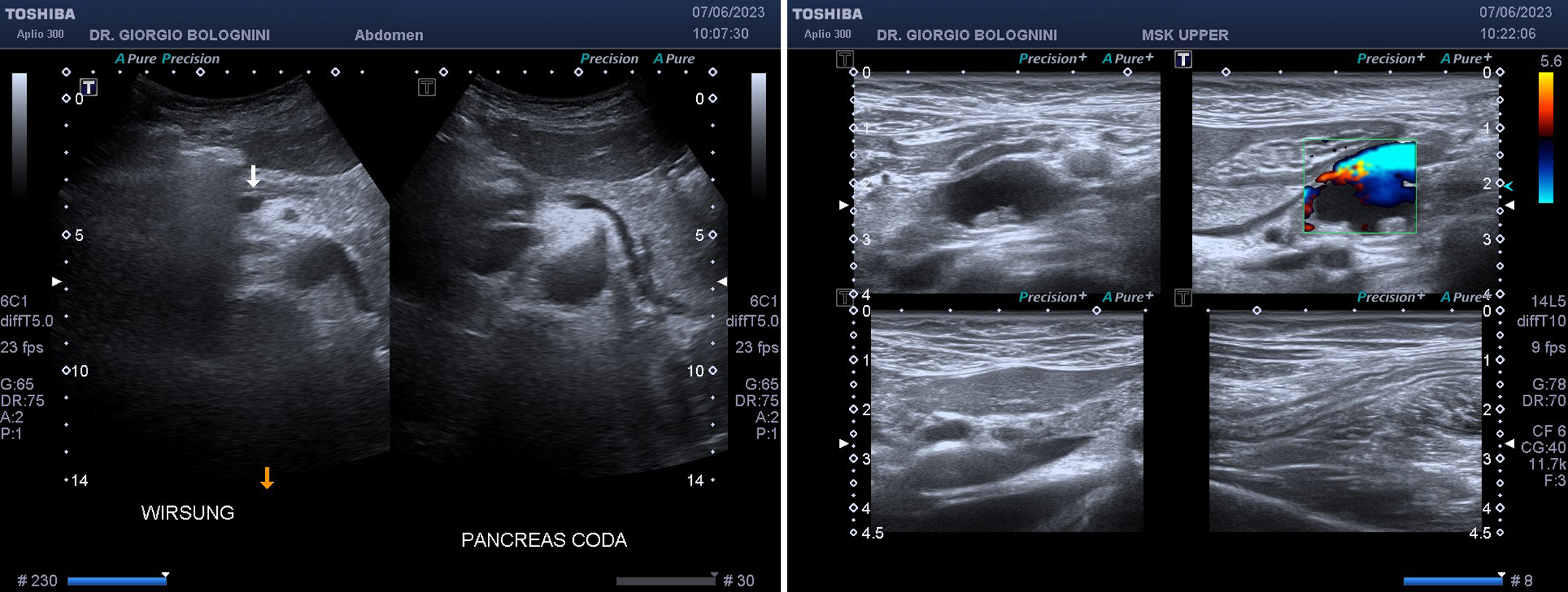
He performs the abdominal MRI which confirms my initial diagnosis, identifying fluid-content formation of the pancreatic hook with maximum diameters of 20x19mm, with thin walls in the absence of contrastographic enhancement after intravenous paramagnetic contrast medium; there are close proximity relationships between the lesion and the accessory pancreatic duct. The finding appears in the first hypothesis to be referable to IPMN of the secondary ducts (Intraductal Papillary Mucinous Neoplasm).
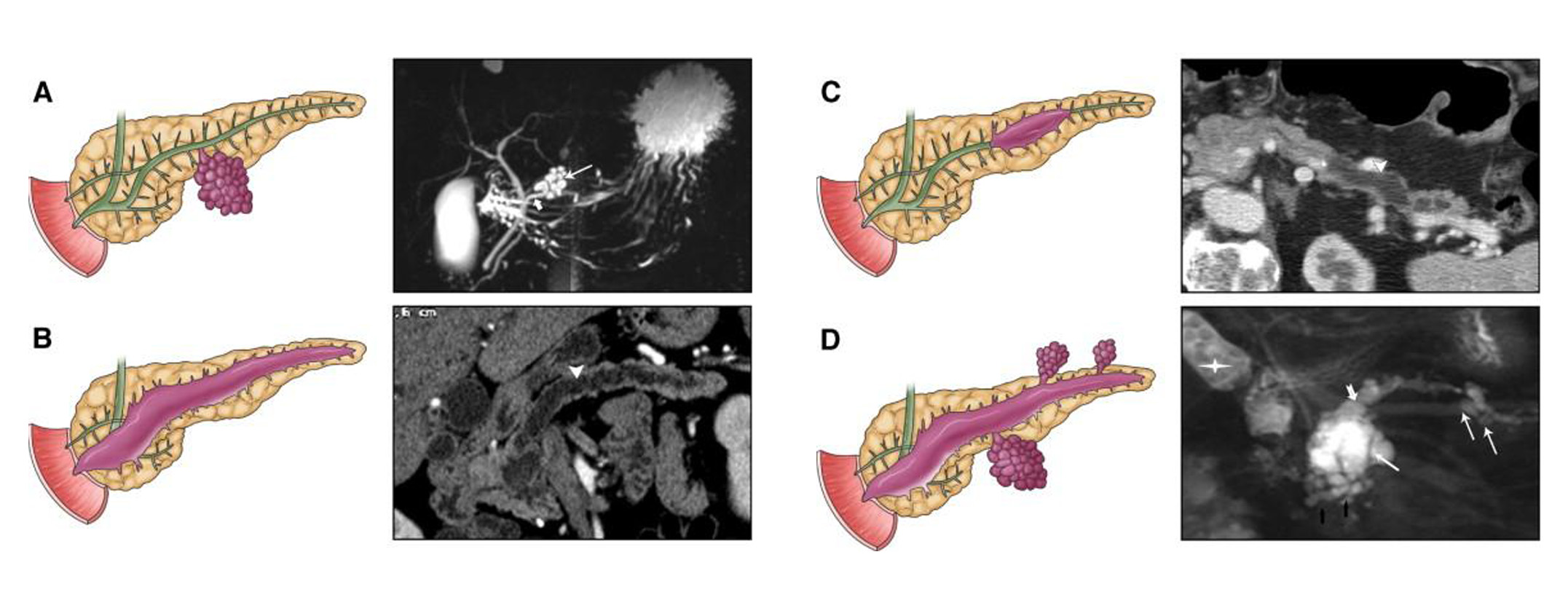
This is a proliferation of mucinous-type cells that form papillary projections inside the pancreatic ducts, so the ducts involved are dilated like cysts and contain mucin; the IPMN MAIN DUCT (MD) which involves the main duct has a high aggressive potential (60-70%) and has a percentage of invasive carcinoma of 40%; the IPMN BRANCH DUCT (BD) which involves the secondary ducts has low-medium aggressive potential (20-25%) and a percentage of invasive carcinoma of 10%, they are often multifocal; the IPMN Mixed Type (MT) has similar aggressiveness to MDs.
IPMNs have a very broad spectrum of biological aggressiveness, from benign to frankly malignant, from adenoma with mild dysplasia to invasive carcinoma. The histological classification of the invasive form is of 3 types: IPMN-TUBULAR CARCINOMA, which arises on papillary epithelium of the gastric and pancreatic biliary type; IPMN-COLLOID CARCINOMA, which arises on intestinal-type papillary epithelium; IPMN-ONCOCYTIC CARCINOMA that arises on papillary epithelium of the oncocytic type.
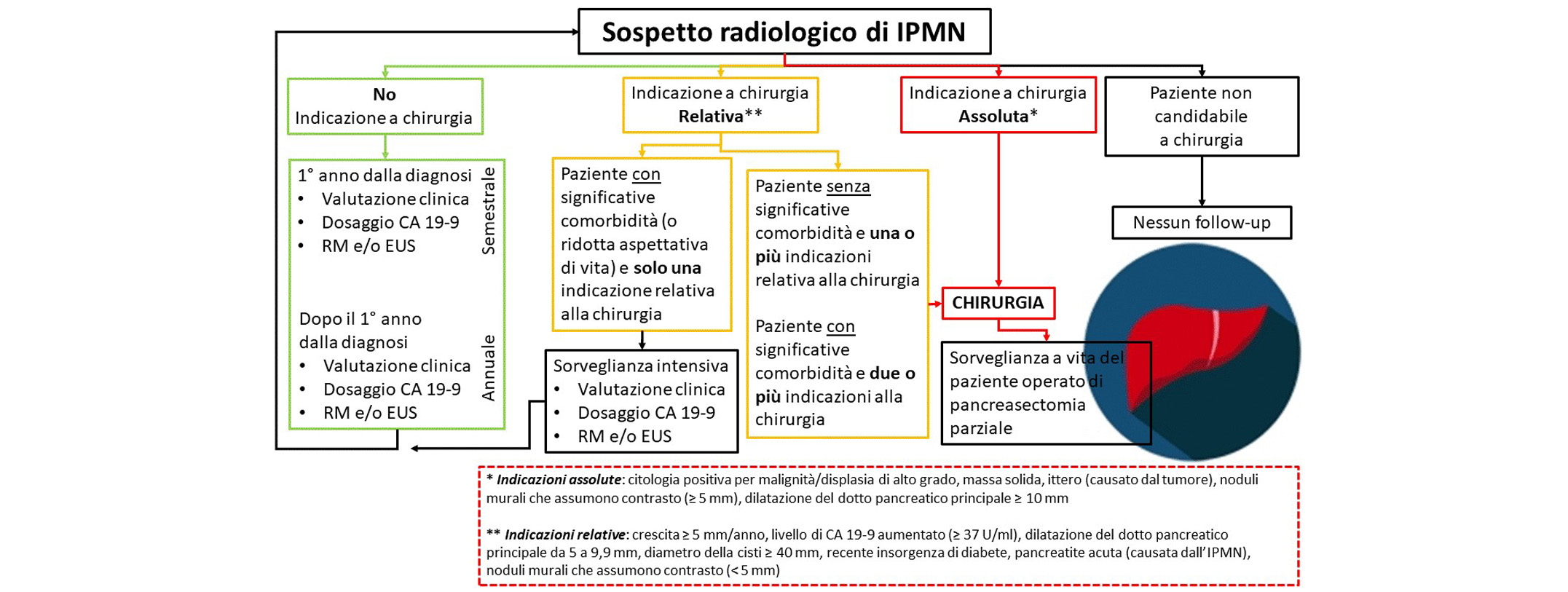
As can be seen upon careful reading, the MRI was unable to identify the two small solid wall formations that I had described on the ultrasound. The patient then on her own initiative decides to hear the opinion of two of the most illustrious Italian pancreas surgeons, Professor Ugo Boggi, Professor of General Surgery at the University of Pisa and Associate Associate in General Surgery at the University of Pittsburgh, and Professor Massimo Falconi, head physician and director of the Pancreas Translational & Clinical Research Center of the IRCCS San Raffaele Hospital in Milan and Professor of Surgery at the Vita Salute University of San Raffaele; both recommend, based on the guidelines, active surveillance of the lesion with cholangioMRI and MRI + contrast medium to be repeated every 6 months for the first two years, following a blood sugar dosage of CEA and CA 19.9, and subsequently in the absence of evolution, cholangioRM and MRI + contrast medium repeat annually, always after dosing CEA and CA 19.9.
The patient then performed an abdominal MRI + contrast medium at 6 months which showed overall growth of the known uncinal cyst, with a diameter of 23x30x27mm (APxLLxCC axes) again without evident communication with the pancreatic ductal system, which appears regular in terms of course and caliber, and without the solid parietal token reported in my previous ultrasound is clearly recognisable. In the meantime, an episode of strong epigastralgia with persistent vomiting occurs, for which the patient visits the emergency room of the San Jacopo Hospital in Pistoia and is subsequently admitted to internal medicine for approximately 10 days for pancreatitis dndd, with CT abdomen + contrast medium which excluded major necrotic-hemorrhagic pancreatitic phenomena or problems of the excretory biliary system.
Once discharged, she decides on my advice to hear a third opinion by consulting Professor Morelli Luca, associate professor of surgery at the University of Pisa, who opts for a re-evaluation of the cyst via ultrasound with contrast medium (CEUS); the ultrasound confirms not only the size of the cyst, but also the presence of the well-known solid parietal tokens previously visualized by me, which seem to pick up the contrast medium.
Professor Morelli Luca at this point opts for an ultrasound endoscopy with FNB cytological sampling, which confirms the solid parietal protrusion of 8mm, proceeding to aspiration of part of the intracystic fluid; the cytological result fortunately excludes the presence of neoplastic cells, resulting in mucin and rare inflammatory cells. However, the patient follows a quarterly ultrasound and six-monthly follow-up with MRI + contrast medium examination.
Bibliography
Ohtsuka T; Castillo C F; Furukawa T; Hijioka S; Jang J; Lennon A M; Miyasaka Y; Ohno E; Sage R; Wolfgang C L; Wood L D International evidence-based Kyoto guidelines for the management of intraductal papillary mucinous neoplasm of the pancreas Journal Article In: Pancreatology, 2023, ISSN: 1424-3903.