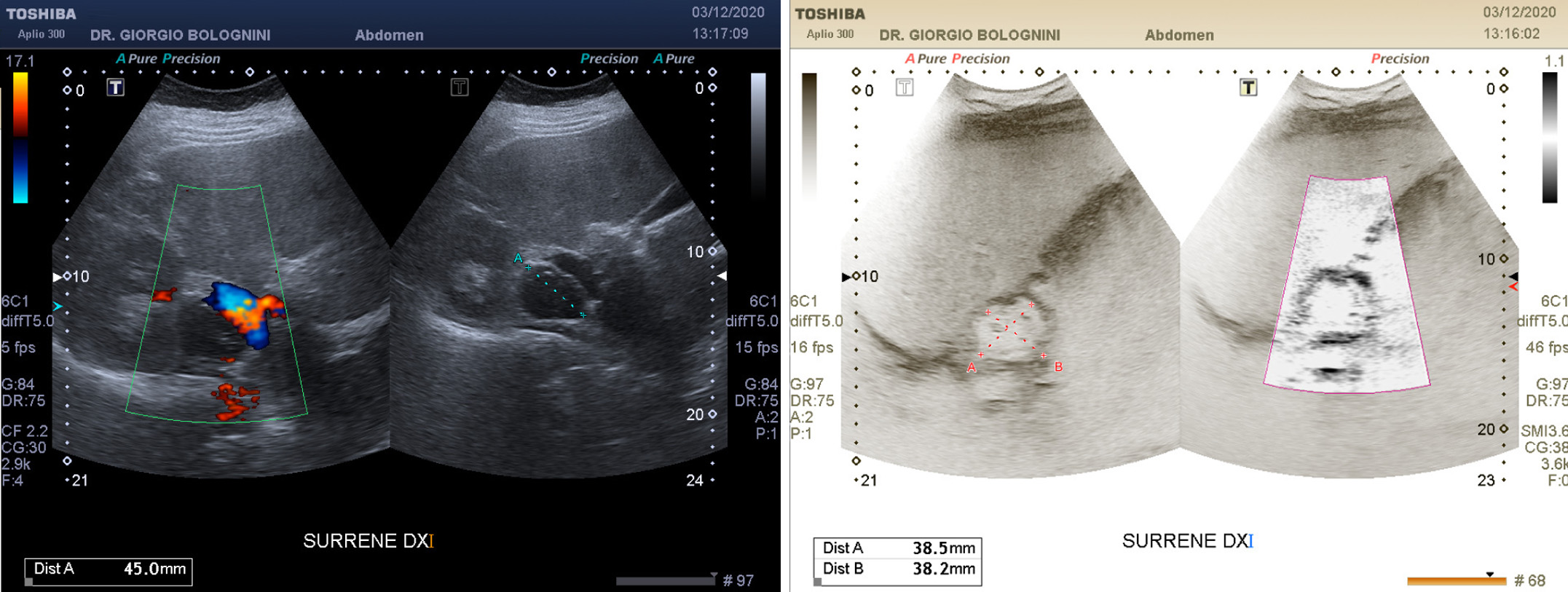
29-year-old girl, at the 22nd week of gestation, previously hospitalized in urology for removal of a right kidney stone with placement of a ureteral stent which was later removed in 2016; goes to the clinic for pain symptoms in the right lumbar region, suggestive of recurrence of renal colic; the ultrasound examination highlights a nodular mass in the right adrenal lodge, approximately 38x40mm, which extends to below the renal vascular pedicle; the formation is substantially roundish, significantly hypoechoic and with internal coarse calcifications; in the Doppler and micro vascular Doppler study no significant internal vascular signals are appreciated. A modest calico-pyelic dilatation of the right kidney is associated, presumably from compression of the pregnant uterus (no obvious stone recurrences).
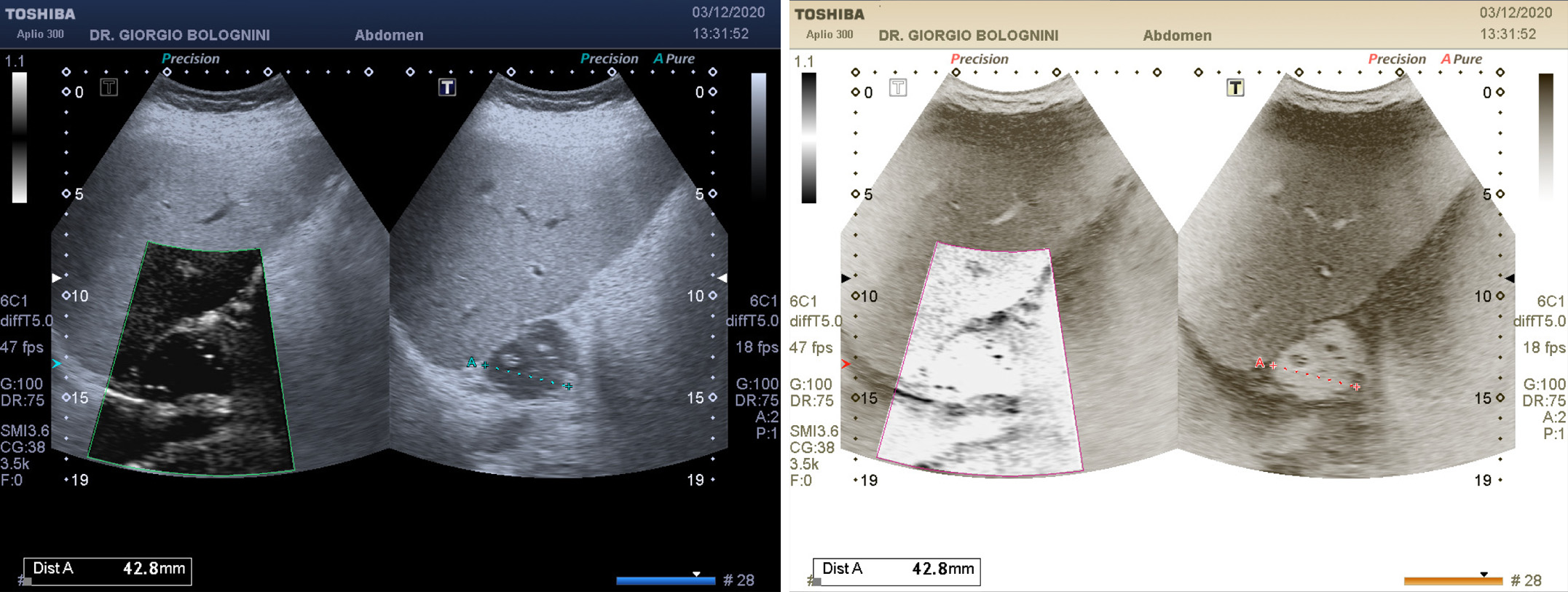
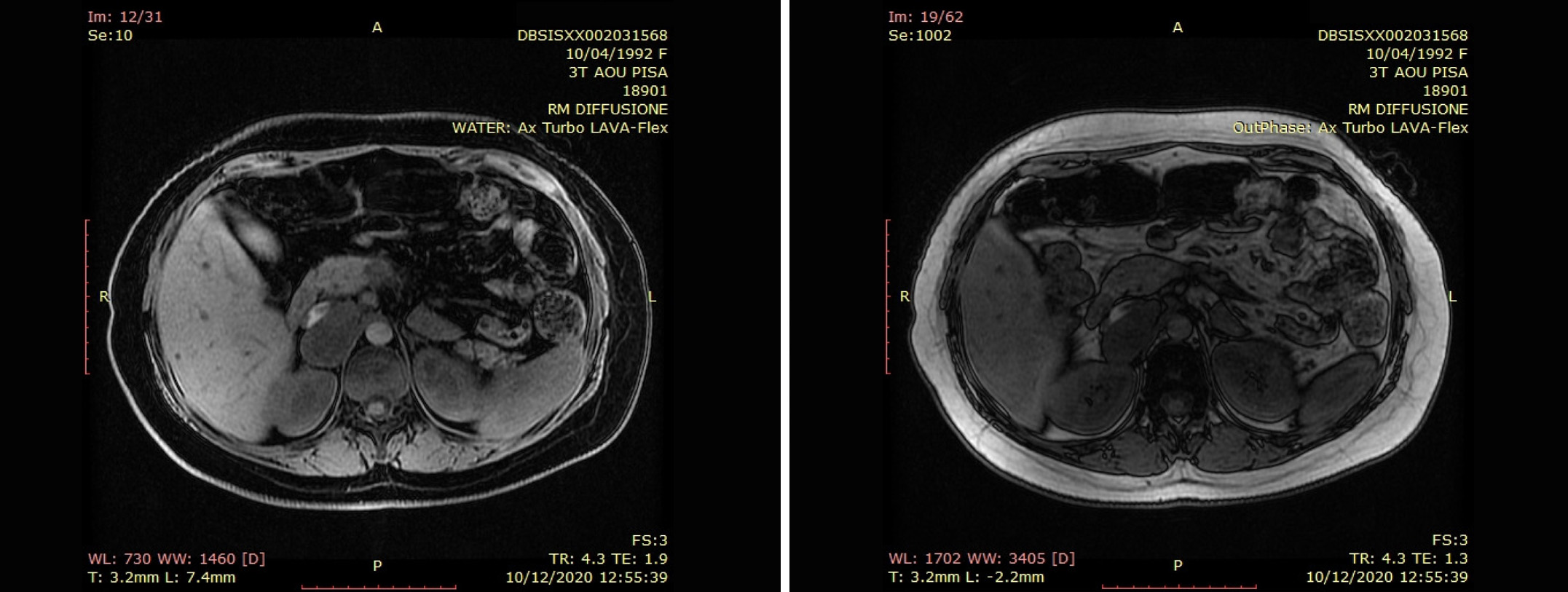
I opt for a referral to the Department of Oncology and Transplant Surgery Division of Cisanello directed by Dr. Alessandro Campatelli for an ultrasound study with contrast, in order to characterize the lesion from a vascular point of view without harming the health of the patient and the fetus. The CEUS essentially confirms the B-Mode ultrasound performed by me, although failing to identify a typical vascularization for adrenal adenomas. Negative urinary metanephrines. The Department therefore requests an MRI of the upper abdomen, which confirms the presence of a lesion of about 53x32mm in correspondence with the right adrenal lodge, which extends retrocavally up to the insertion of the left renal vein; this lesion shows expansive behavior, dislocating and compressing the inferior vena cava, which remains patent, and is placed against the right adrenal gland, which however seems to keep its structure intact; there is also a further rounded solid formation of about 15mm caudal to the first lesion, immediately below the origin of the right renal artery; these lesions have a homogeneous solid structure and the larger one has a pseudocapsulated appearance, absence of adipose content and significant restriction of proton diffusivity; the formations can therefore be compatible with ganglioneuromas.
In agreement with the patient and under strict clinical laboratory monitoring, the surgical team of prof. Luca Morelli of the SD General Surgery 1 Univ Osp Cisanello Pisa (director Prof. Di Candio Giulio) decides to plan the operation after the birth; Two weeks after delivery, the patient underwent robot-assisted removal of retrocaval and paracaval lesions suggestive of ganglioneuroma and ganglioneuroma fragments. The subsequent histology performed at the external network of the rare tumor center is conclusive for encapsulated mesenchymal neoplasia without significant atypia consisting of proliferation of spindle elements interspersed with mature ganglion cells and with focal areas of hyaline sclero-like appearance, in the absence of areas of necrosis, therefore compatible with the diagnosis of extraadrenal ganglioneuroma.
The patient is in current well-being, and follows an annual ultrasound follow-up.