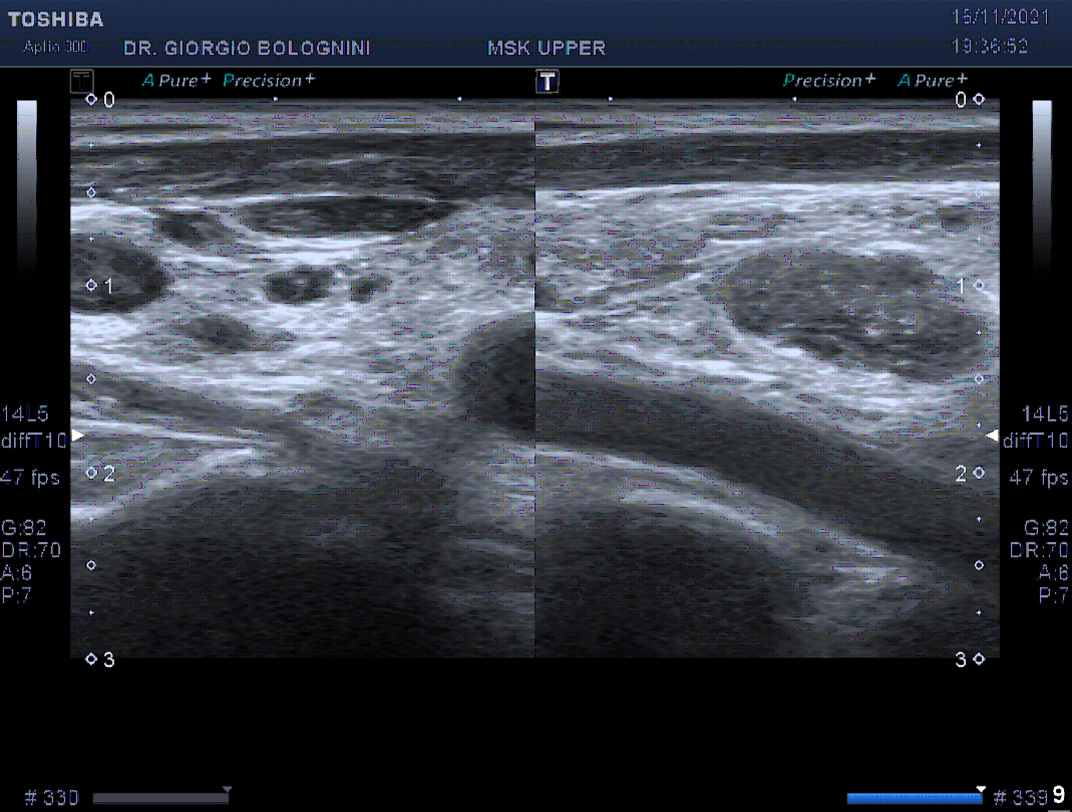
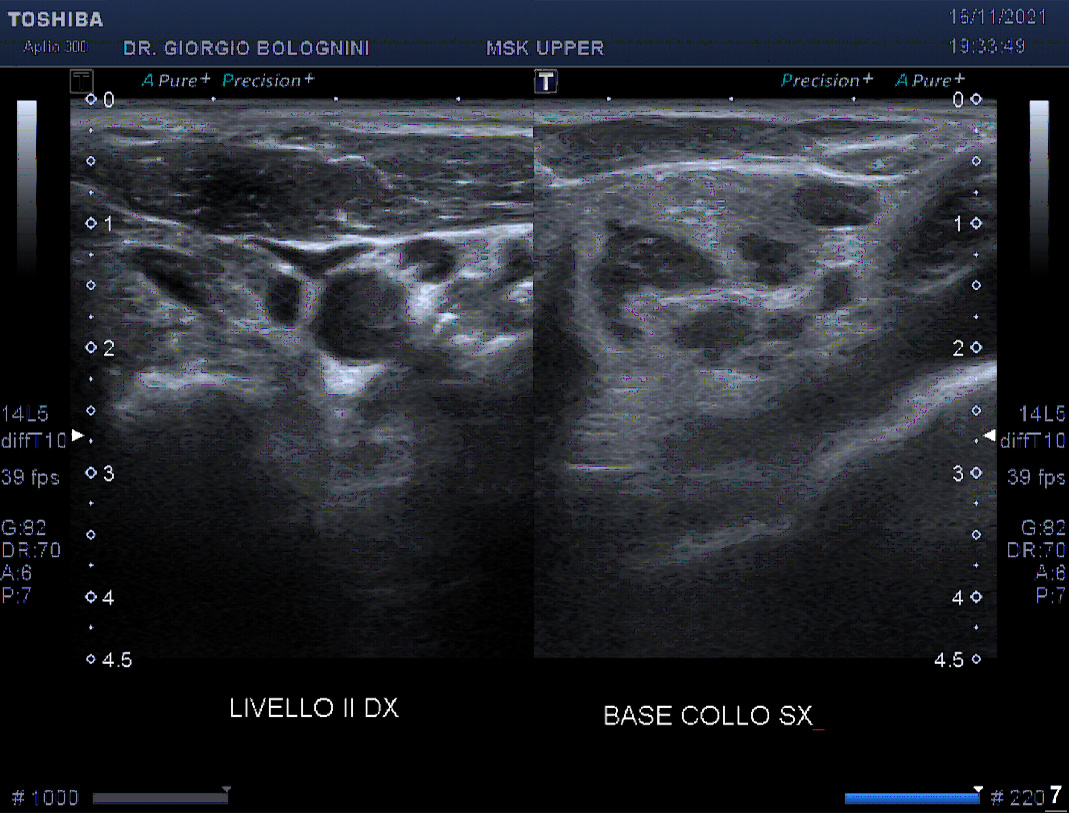
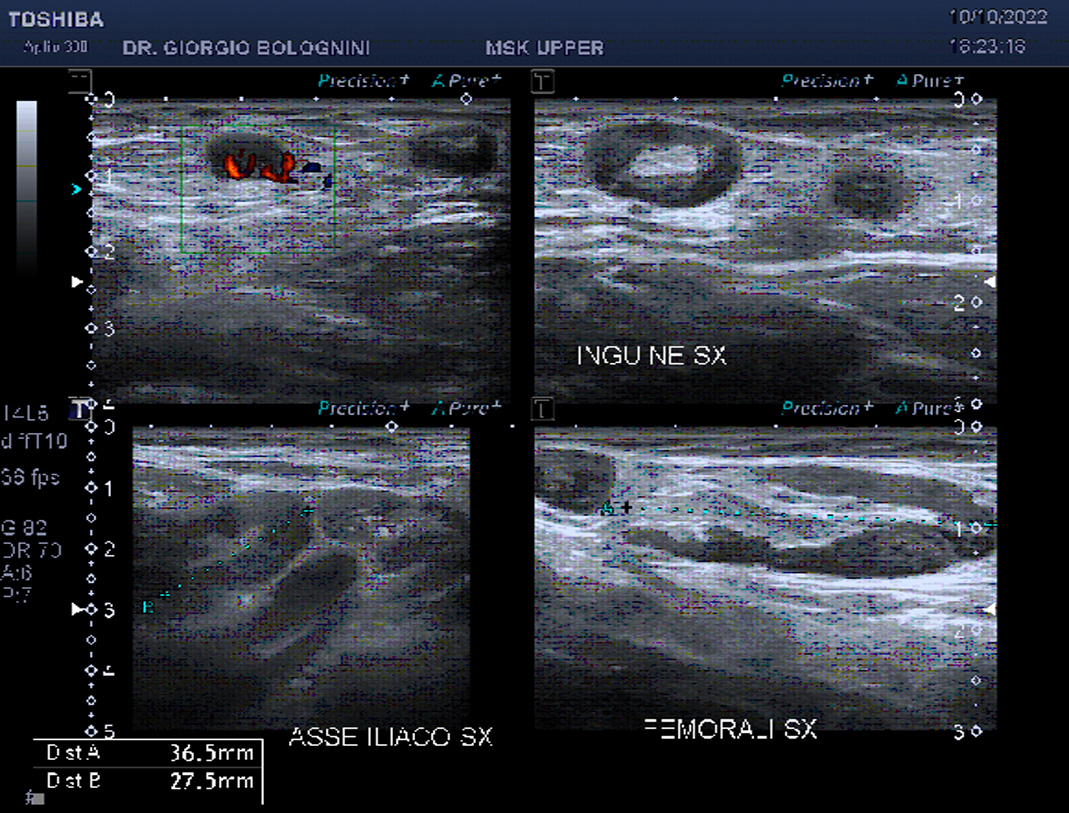
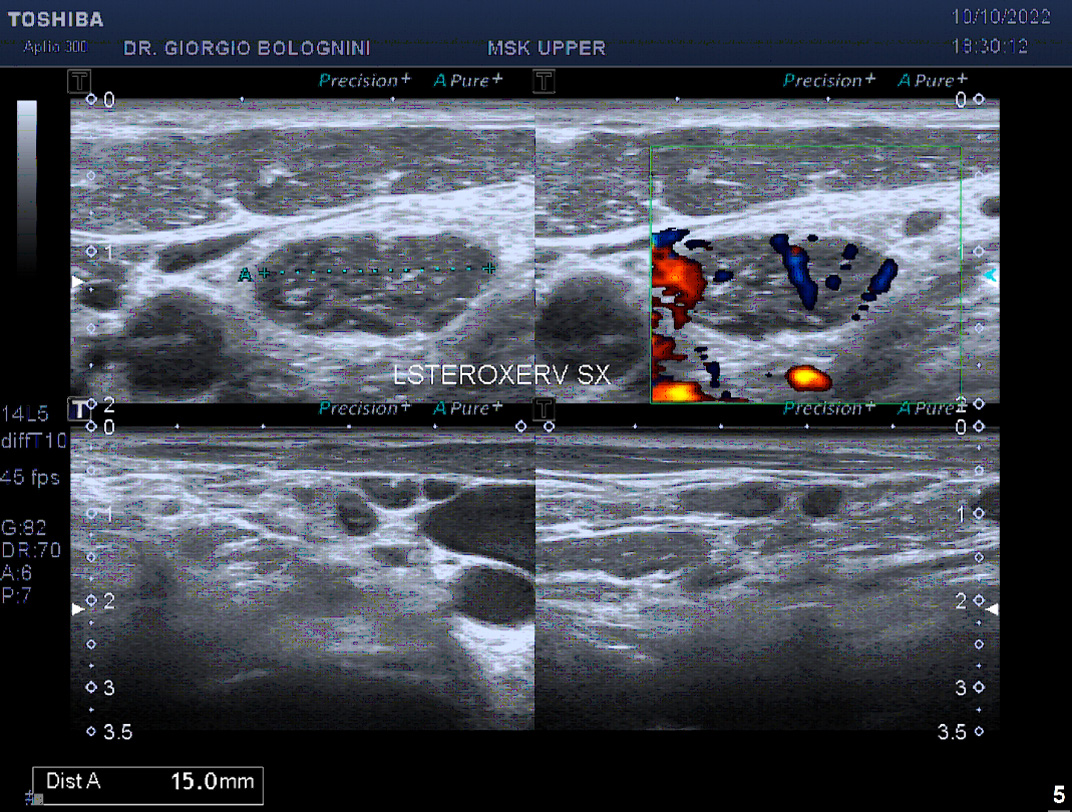
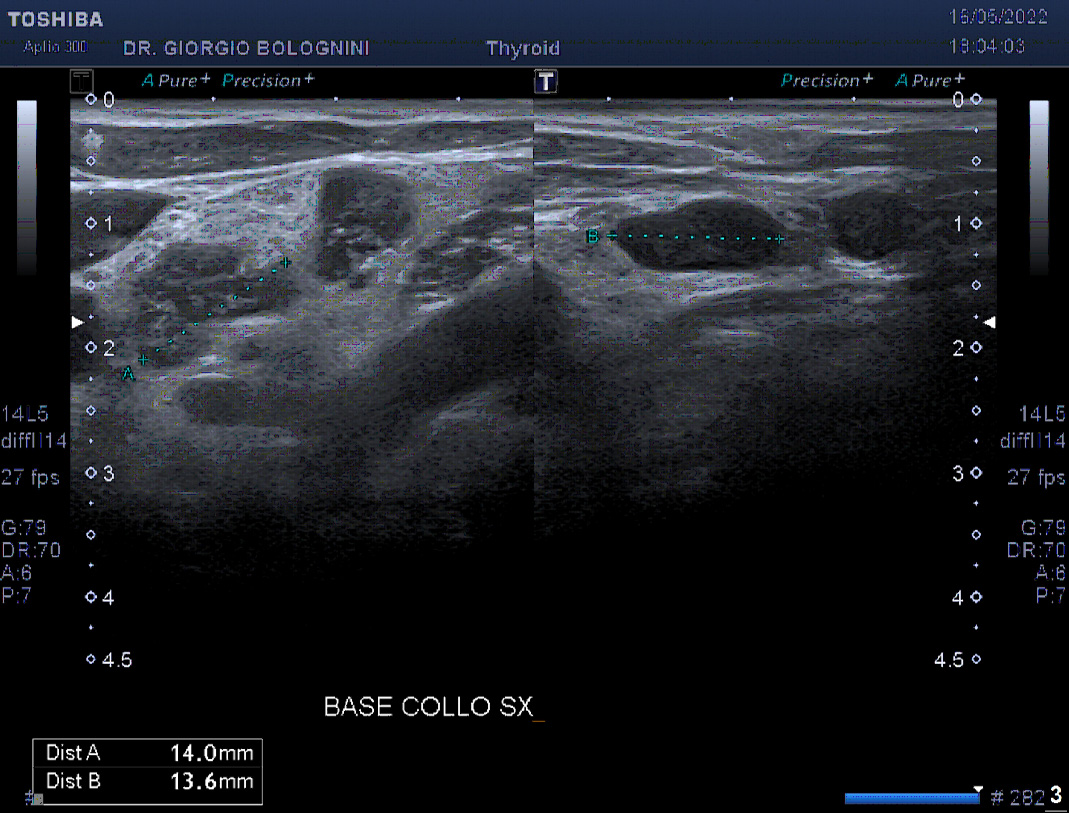
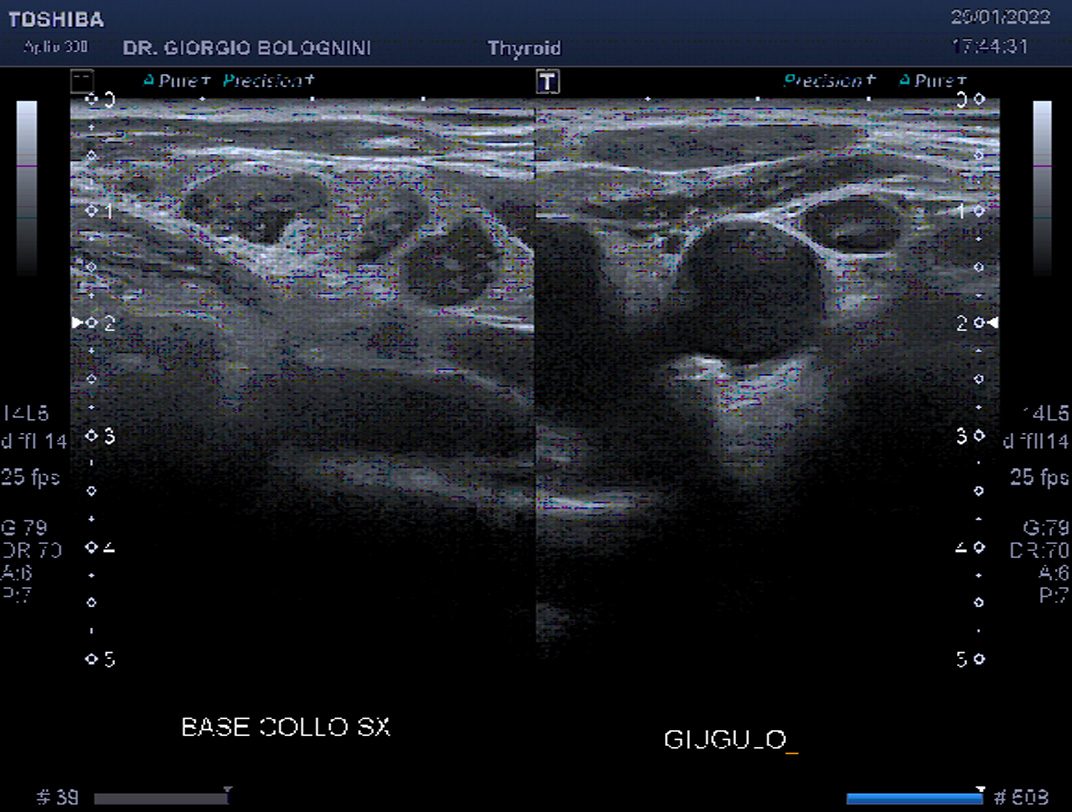
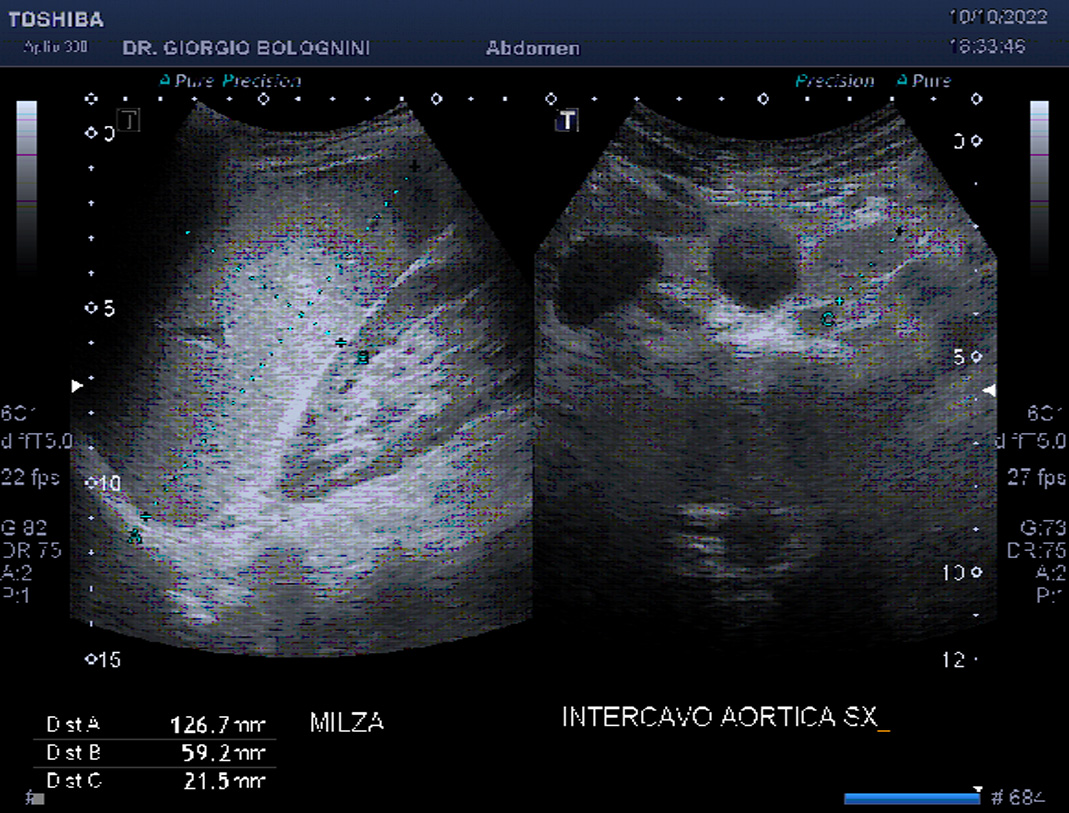
54-year-old man in clinical well-being and not affected by chronic pathologies, ex-smoker, sporty, slender with BMI 22, no significant family history of oncological diseases; operated on the supraspinatus tendon of the left shoulder; comes to the clinic for a post-operative shoulder check-up. The examination shows a periosteal remodeling irregularity of the humeral foot print as a possible cause of persistence of shoulder pain, with the supraspinatus tendon substantially intact. It is also identified as a collateral finding of multiple lymphadenopathies with a border line ultrasound appearance in the subclavicular area (with the largest being approximately 22mm with absence of hilus and a 'starry sky' appearance), in the ipsilateral axillary area (with the largest being hypoechoic and roundish of approximately 12mm), at the base of the left neck (lymph node package tending towards confluence) and at levels III and II with small, markedly hypoechoic and rounded lymph nodes. Sporadic similar lymphadenoapties are also identified in the right subclavicular and axillary areas and also in the abdomen in the para aortic and para iliac areas, with the largest being 19mm. Spleen within dimensional and ecostructural limits (diameter of 11x5.6cm). At the inguinal level, similar nodal enlargements are found, with a thickened hypoechoic cortex, however with a hyperechoic central hilum still clearly identifiable.
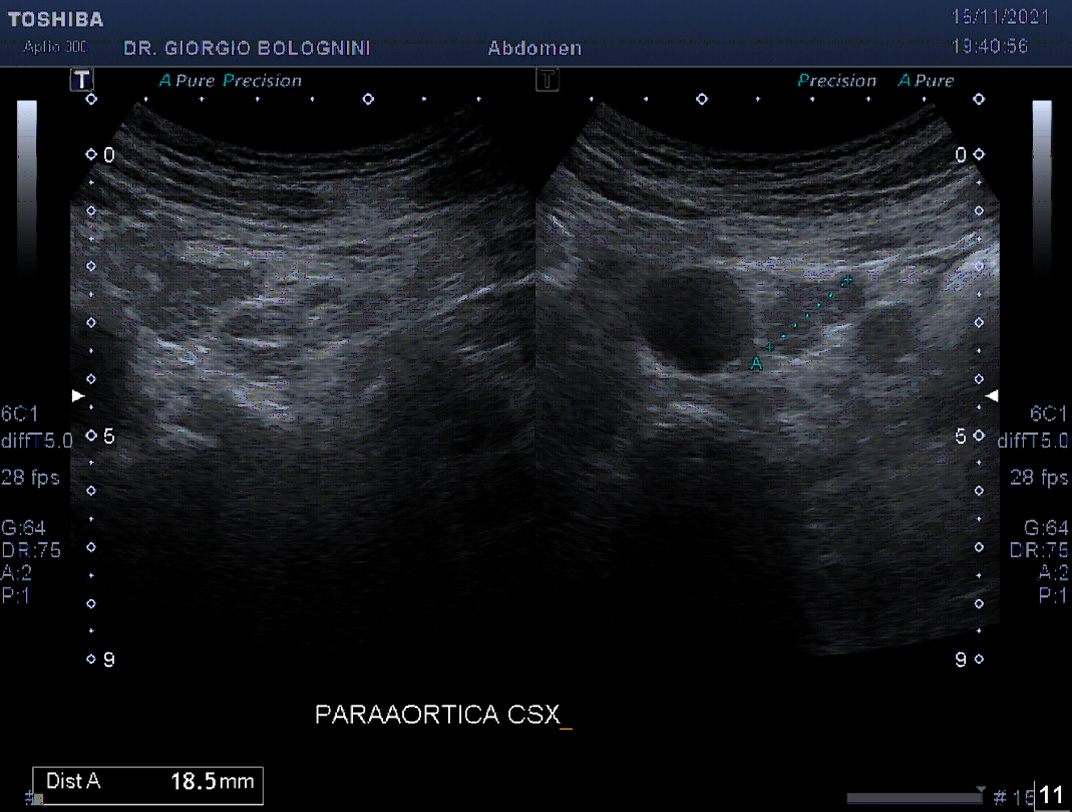
I suspect a primary lymphatic disease, I send him to the hematology department of the Pescia hospital where the patient receives a first visit approximately three months after the ultrasound; here he performs complete blood tests (normal, with: WBC 5.83 with respected formula; ves 3, PCR 0.4), a CT neck chest abdomen + contrast medium which shows the presence of multiple mediastinal lymph nodes of maximum 18mm, mild splenomegaly (longitudinal diameter of approximately 13cm), at the abdominal level in the lumboaortic area and in the bilateral inguinal area numerous pathological lymph nodes, the largest in the left para-aortic area of maximum 28mm tending towards confluence. Similar pathological lymph nodes are reported in bilateral laterocervical cases. He then performs a total body PET which shows the presence of multiple LAPs with a maximum SUV of 6.2mm, also in the diaphragmatic, abdominal and colonic walls. While waiting to undergo an excisional biopsy of the major left supraclavicular lymph node and with approximately six months having passed since the first ultrasound check-up, the patient returns to my ultrasound clinic for a re-evaluation of the lymph node disease, following a new check of the blood tests, which again show a normal picture (GB 6.53, N 66.9, L 18.5, ves 7, pcr 0.18, ldh 135).
The ultrasound shows an overall growth of the major lymph nodes, in particular in the left axillary cavity, and a greater destructuring of them, with complete disappearance of the hilum also at the level of the inguinal lymph nodes, and fine internal hyperechoic trebeculature. The vascularization of the major lymph glands appears frankly aberrant, centripetal and multi-focal. Therefore, in general, ultrasound shows progression of the disease in the superficial lymph node stations.
Upon histological review of the surgically excised lymph node in the left supravlaviar, the result is MANTLELAR LYMPHOMA common variety SOX11+, ki67 20%, stage IV due to localization also in the colon and bone marrow. The patient is then listed for an autologous marrow transplant and subsequent maintenance therapy with rituximab.