22 year old patient not suffering from chronic pathologies, with negative family history of abdominal pathology; goes to the emergency room for acute abdominal pain; the appropriate laboratory tests are carried out which are all normal, and a negative abdominal ultrasound, with evidence of suspected angiomyolipoma in the left kidney. The pain passes with the appearance of the endometrial cycle. After about a month he goes to my clinic for a level II ultrasound study on the suspected angiomyolipoma. During the abdominal ultrasound I am going to confirm the presence of the renal angiomyolipoma on the anterior margin of the left kidney, measuring approximately 15x14mm, not causing compressive effects on the surrounding venous circulation, but I am also going to identify a saccular dilatation of the retropancreatic arterial vessel, to the right of the tripod, therefore presumably affecting the hepatic artery, with maximum DAP of approximately 16mm and presence of turbulent flow. Also evidence of two macrocalculi of the gallbladder, not causing locoregional complications nor significant dilation of the biliary excretory system.
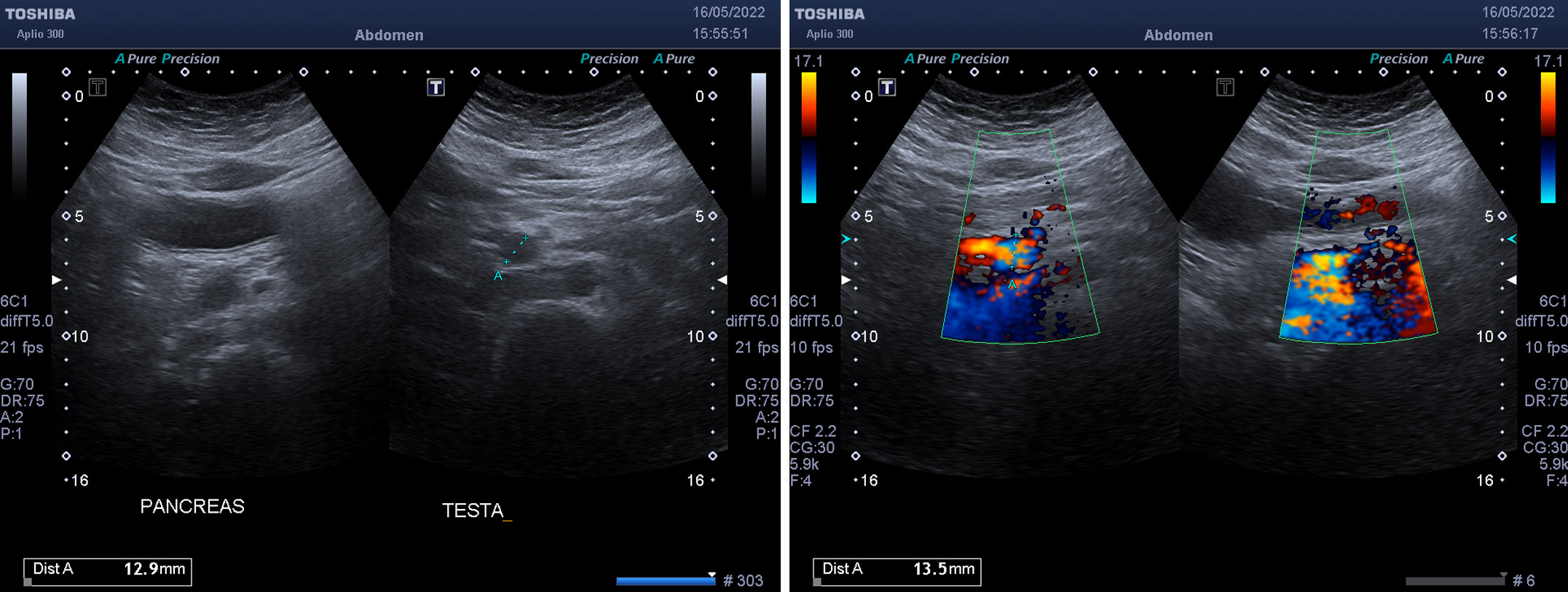
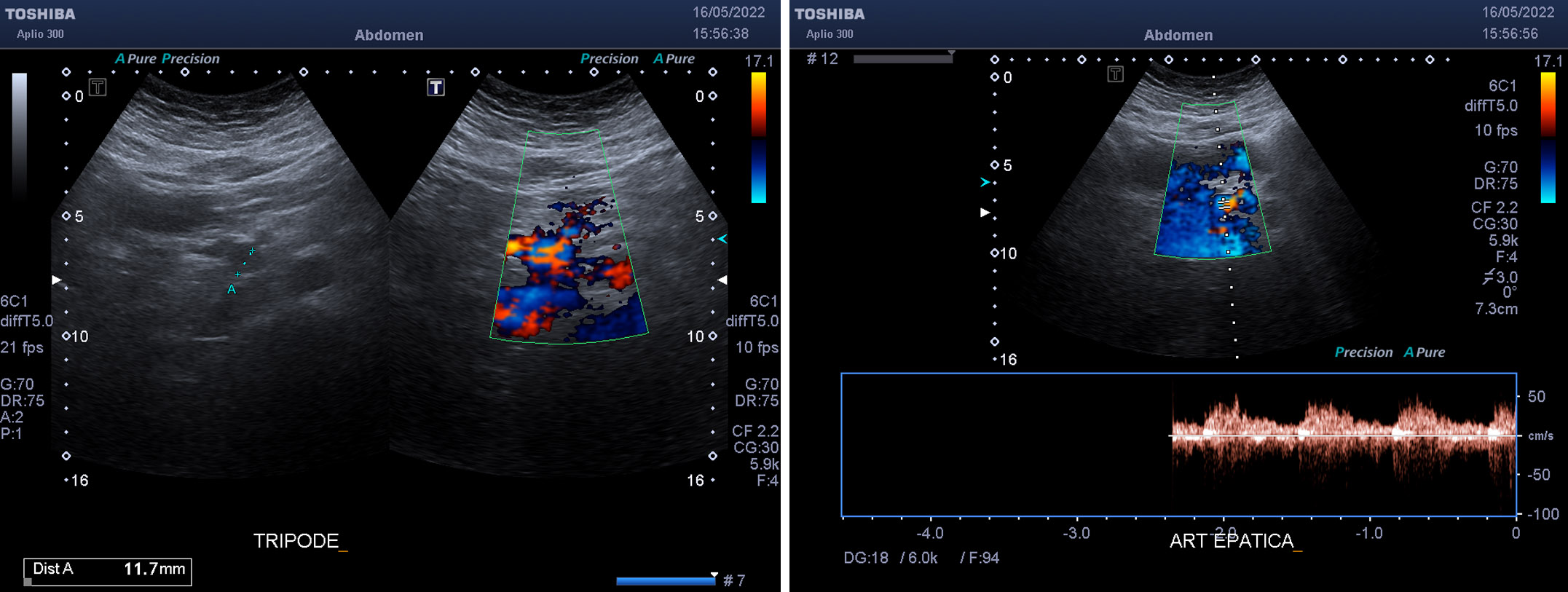
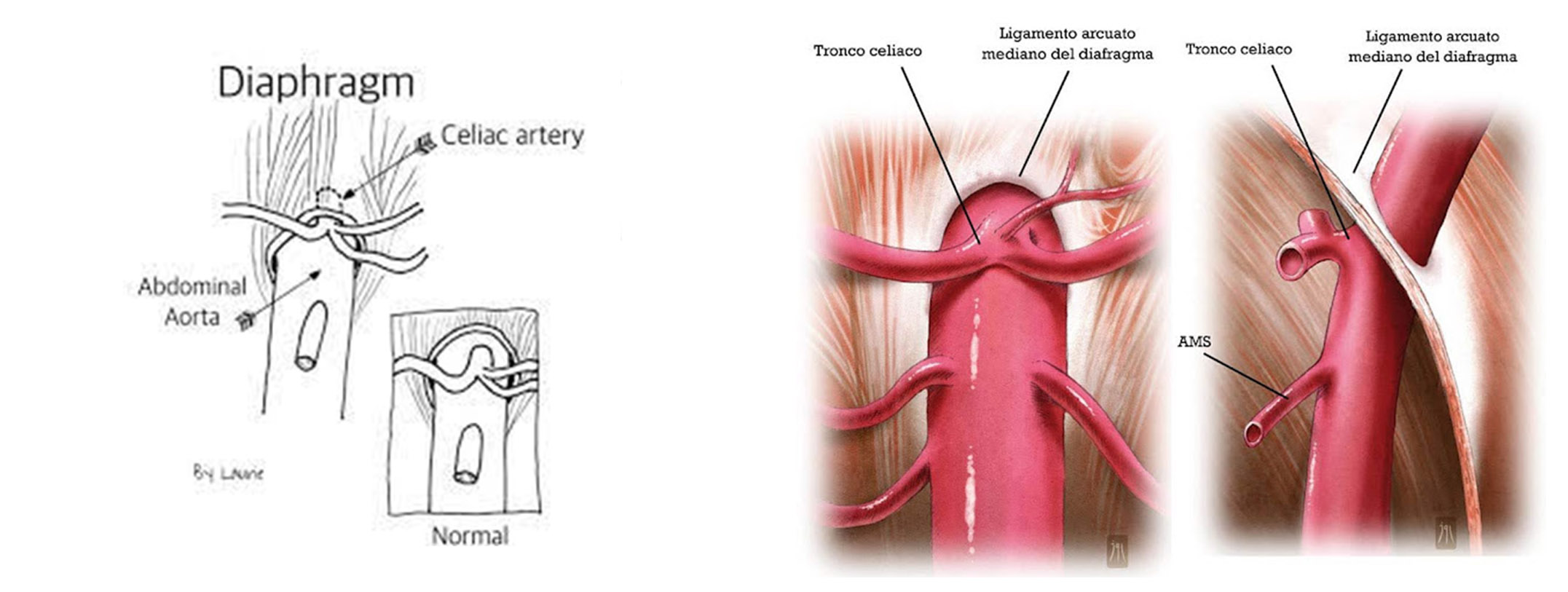
I then advise the patient to undergo an abdominal MRI with contrast medium which reported the presence of an oval formation of approximately 16mm in correspondence with the postero-medial portion of the uncinate process of the pancreas, posterior to the portal vein and lateral to the superior mesenteric artery. of maximum diameter of a vascular nature presumably pertaining to the proximal portion of the hepatic artery, of an aneurysmal dilatation type. A CT angiography was then performed which reported the presence of a celiac trunk of slender caliber and filiform at the origin due to steno-obstruction, with post-stenotic segmental dilatation of a maximum caliber of 8mm, regularly canalised downstream, with development of hypertrophic circles of pancreaticoduodenal recanalisation at origin from the superior mesenteric artery; presence of saccular aneurysmal dilation with non-calcific walls with maximum diameters 16x13mm APxLL originating from the inferior pancreaticoduodenal, in the absence of thrombotic apposition of the sac; superior mesenteric artery of caliber within limits, the splenic portal venous axis is patent. To complete the diagnostic tests, the patient underwent Doppler ultrasound of the visceral vessels which showed stenosis of 60% of the origin of the celiac artery and stenosis of 60% of the origin of the superior mesenteric artery, determined by extrinsic compression of the arcuate ligament of the diaphragm during breathing; presence of visceral aneurysm of the inferior pancreaticoduodenal artery, uncomplicated and unchanged in size. A final diagnosis was therefore made of Dunbar syndrome, a rare medical condition that occurs when the celiac artery, a major blood vessel that supplies blood to the upper abdominal organs, is compressed or narrowed due to compression of the median arcuate ligament (a fibrous band of the lower margin of the diaphragmatic dome); this compression can lead to abdominal pain typically postprandial, nausea, vomiting, weight loss, diarrhea; it is often due to anatomical variations (genetically determined) in the position and orientation of the celiac artery and the median arcuate ligament.
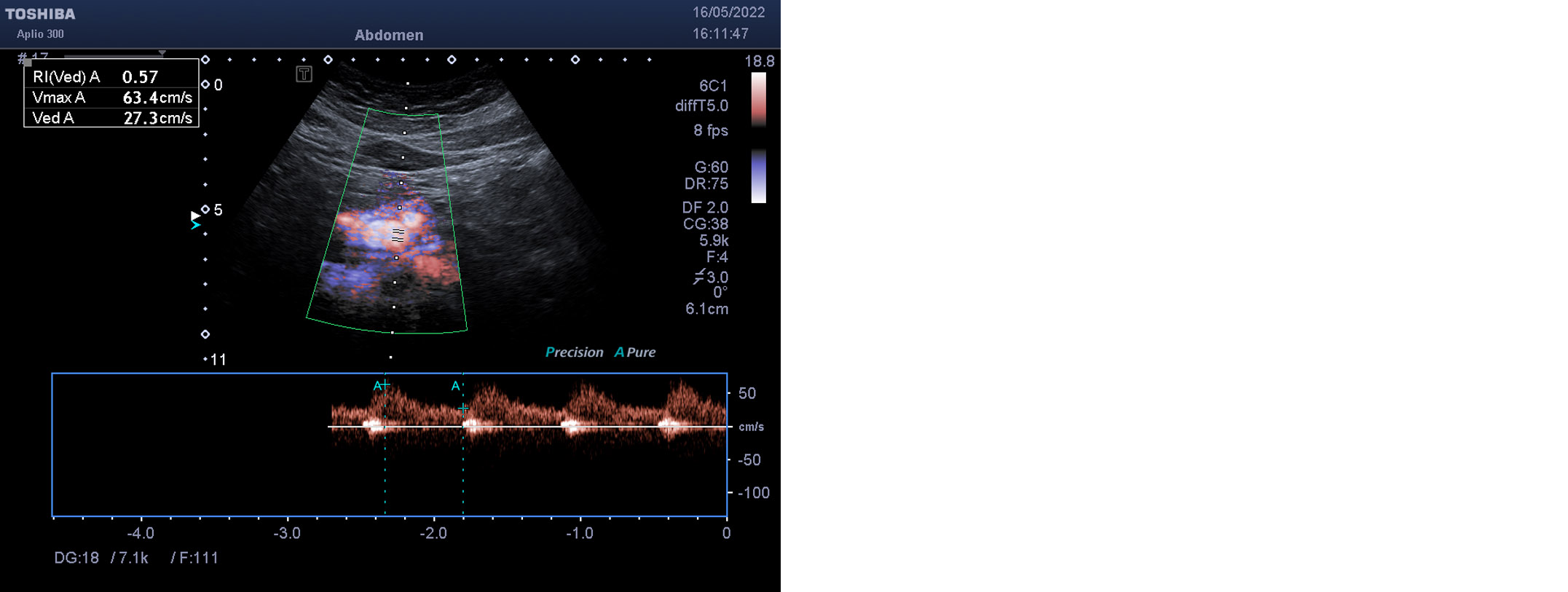
The patient was therefore admitted to the University General Surgery 1 of Cisanello Pisa, director Prof. Morelli Luca underwent robotic arcuate ligament section surgery and robotic cholecystectomy; the operative course was uneventful. The subsequent Doppler ultrasound of the visceral vessels revealed the absence of significant stenosis of 60% of the origin of the celiac artery, with a sprinter S\D = 421\61 cm\sec during the entire respiratory cycle; patent superior mesenteric artery, with S\D velocity 356\58 cm\sec; the visceral aneurysm of probable origin from the inferior pancreaticoduodenal artery, saccular, adjacent to the proximal portion of the superior mesenteric artery, of 15mm DAP, is stable, without direct signs of parietal thrombosis.
The patient, currently in full health, undergoes six-monthly ultrasound checks to evaluate the size and morphology of the hepatic artery aneurysm which did not require preventive stenting.