- Dott. Giorgio Bolognini
- Clinical Cases
- Mar 2024
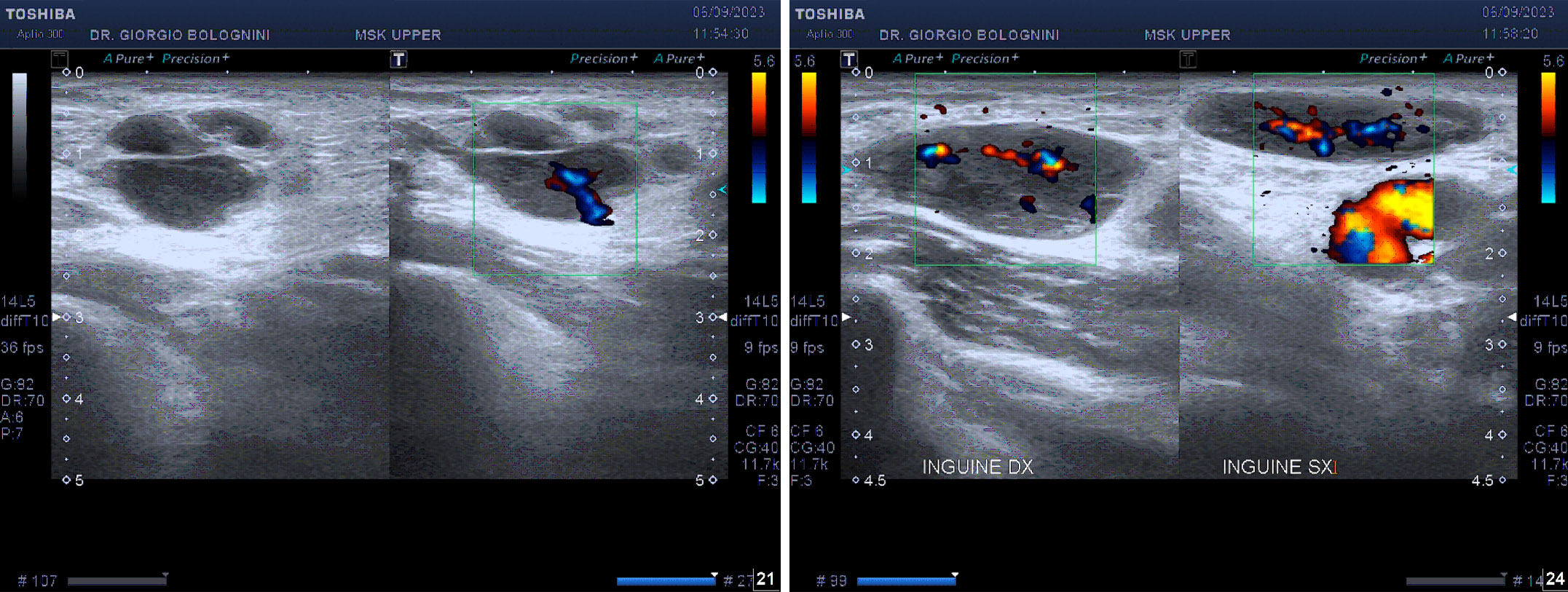
CASE 16 - FOLLICULAR LYMPHOMA
80-year-old patient who underwent right inguinal hernioplasty and coronary angioplasty, suffering from transitional prostatic hypertrophy; a brother who underwent surgery for intestinal lymphoma; for a right inguinal swelling at the site of the previous operation, carry out an ultrasound of the superficial tissues at another site, which detects lymph glands with a frankly evolving appearance. He carries out an initial haematological examination in which there are no particular alterations in the blood tests, in particular the electrophoretic trace is regular. At three months he was sent to my ultrasound clinic for a second level lymph node ultrasound; the examination shows that the well-known inguinal lymph nodes visualized in previous ultrasound scans, while maintaining a substantially centrifugal central vascularization, take on a packet-like morphology with destructuring of the cortex (peripheral hyperechoic clods), with fine internal trabeculation suggestive of primary lymphatic disease. The largest measures approximately 32mm in long axis. The picture at the level of the left groin is similar, where however no packets are found, and at the two axillary cables, where the largest lymph node on the left measures approximately 15mm on the long axis. Another similar 13mm lymph node is found at the base of the left neck. The remaining laterocervical lymph nodes have a more reactive appearance
I therefore recommend that the patient undergo a new specialist haematological evaluation to carry out an excisional biopsy on the major lymph node in the right inguinal region; the result of the biopsy is the following: lymphoma derived from peripheral B lymphocytes of the follicular center (follicular lymphoma) with follicular architecture grade 3a, with immunophenotype CD20+, CD10+, blc 6+, bcl 2+, cyclin D1-, CD23-, CD3-, CD5-, MIB-1 40%. The total body CT scan with contrast medium shows the presence of multiple lymphadenopathies at the level of the axillary and abdominal para-aortic and intercavoaortic stations, in the bilateral iliac site, confluent in the common iliac site and with a maximum short axis of 20mm in the external iliac site. Spleen normal. The total body PET exam highlights pathological uptake of the radiopharmaceutical in the left retroclavicular lymph node (SUVmax 3.4), bilateral axillary (SUVmax on the right 4.8, on the left 4.5), at the level of the left internal mammary chain (SUVmax 2.1), in the intercavus- aortic (SUVmax 4.2), in left para-aortic (SUVmax 4.3), in bilateral common perioliac (right SUVmax 6.7), in bilateral external iliac (right SUVmax 6.3, left SUVmax 3.6), in bilateral obturator (right SUVmax 6y.4, left SUVmax 4.1) and in bilateral inguinal (SUVmax right 6.1, SUVmax left 4.7).
The final diagnosis is therefore grade 3 follicular lymphoma, stage IIIA (although in the absence of medullary evaluation), MIB-1 40%.
Given the age of the patient and his good clinical conditions, in accordance with the GELF criteria, the patient is placed under close observation with quarterly evaluation including complete blood chemistry tests and ultrasound examination of the abdomen and lymph node stations.
The last total body ultrasound check shows destructured lymph nodes in the right groin, confluent in a packet, with the largest of approximately 35 mm, equipped with aberrant vascularization and peripheral hyperechoic clods, with fine internal trabeculation. The pathological lymph nodes in the left groin and along the iliac axes are less evident. The left major axillary lymph node is markedly destroyed and hypoechoic, measuring approximately 25mm, with peripheral areas of aberrant vascularisation. Pathological lymph nodes are also reported in the right axillary, bilateral subclavicular, and left supraclavicular areas, where we find a destructured and hypoechoic lymph node of approximately 15mm. The major laterocervical lymph nodes are still visible at the hilum.