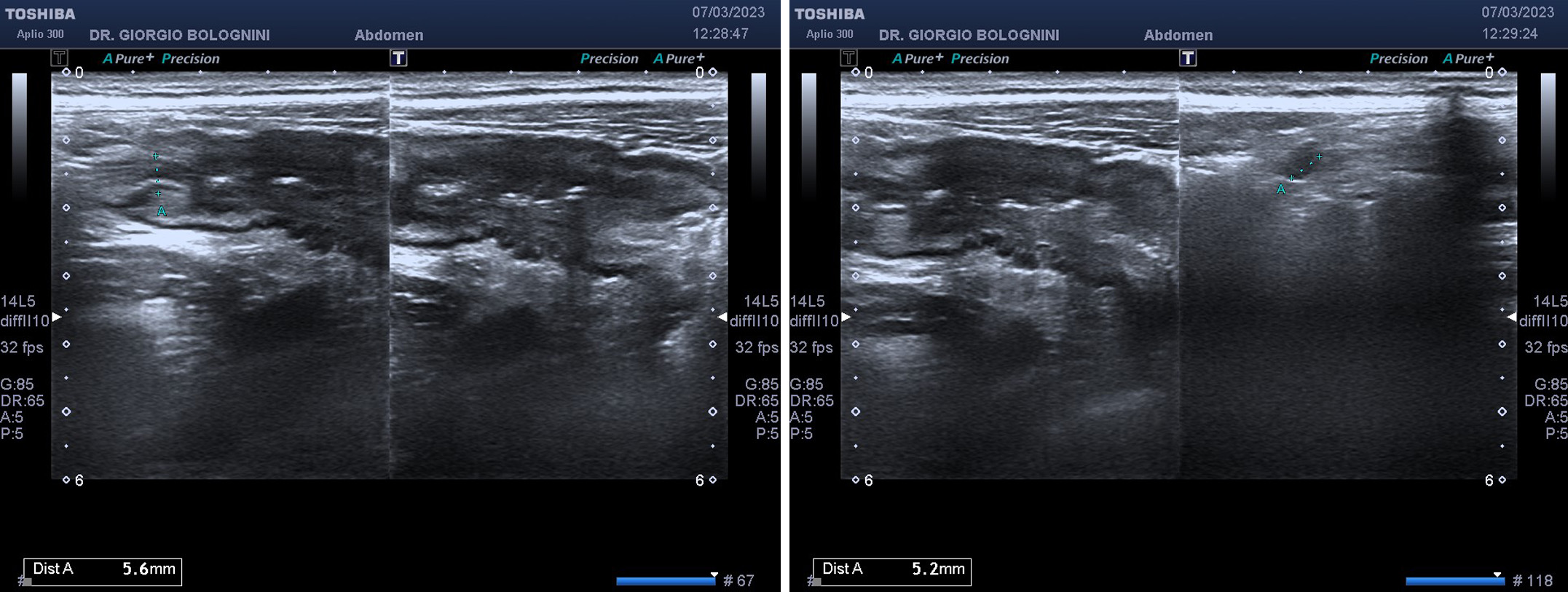
32 year old girl, nulliparous, with a father suffering from chronic erosive gastritis; repeated episodes of watery diarrhea associated with pain in FID and sporadic emulsion of reddish mucus, which have occurred over the past few months with increasing frequency; blood tests showing modest neutrophilic leukocytosis and ves at the upper limits of normal; decrease of approximately one point in hemoglobin compared to the control of the previous year, despite the absence of anemia. He has been going to my ultrasound clinic for acute abdominal pain associated with constipation for about 4 days. On ultrasound I detect a marked hypoechoic thickening of the walls of the terminal ileum, with a section of the viscera measuring 16 mm and signs of arterial hypervascularisation with low resistance indices; significant reduction of the lumen in the pre-valvular area.
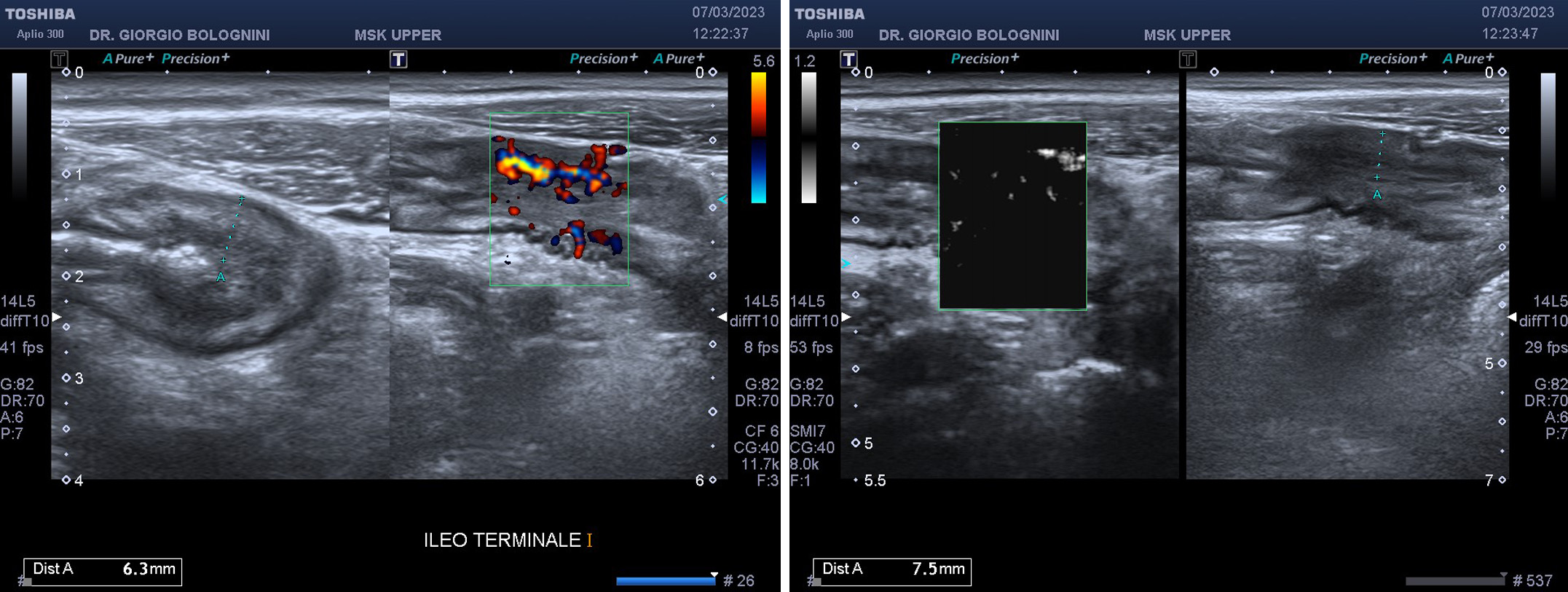
I immediately suspect terminal ileitis of possible autoimmune origin similar to Crohn's disease due to the sectoral localization found, for which I request the dosage of fecal calprotectin and recommend performing a diagnostic ileocolonoscopy.
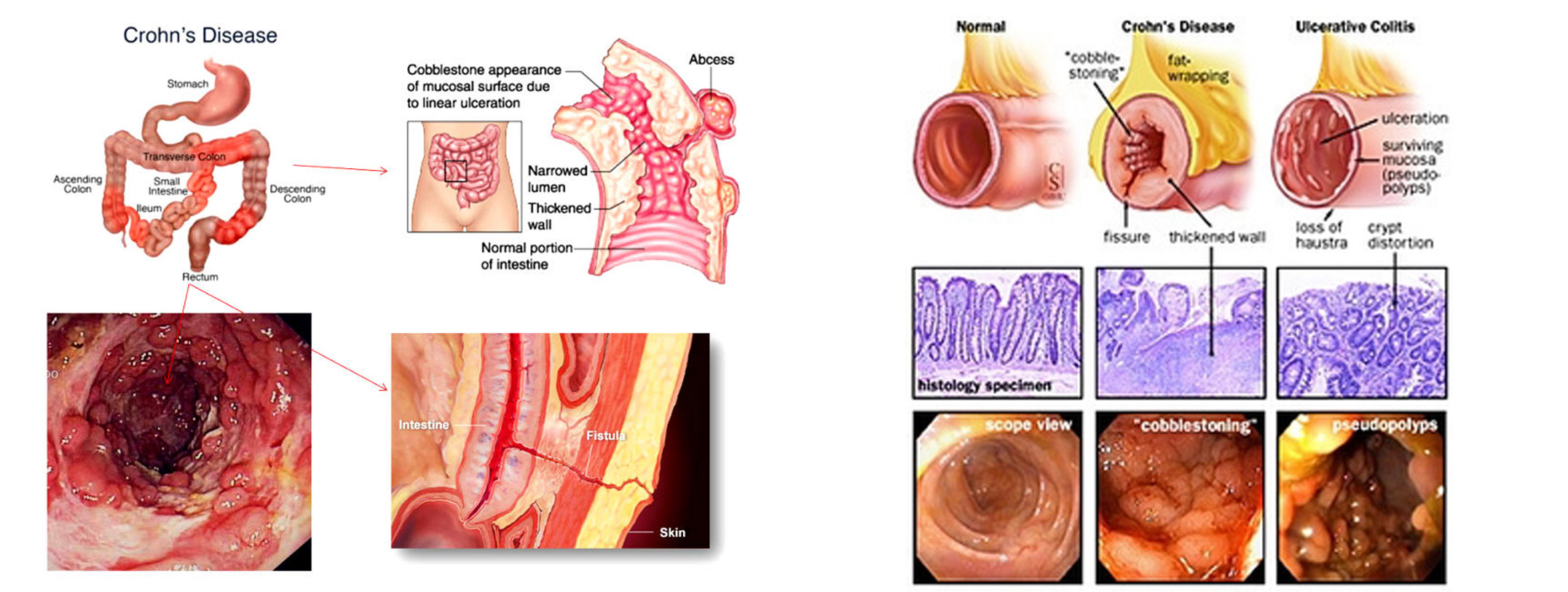
Crohn's disease begins with inflammation and cryptic abscesses that progress to small, focal aphthoid ulcers. These mucosal lesions can become deep, longitudinal and transverse ulcers, with mucosal edema that gives the intestine a characteristic cobblestone appearance. Transmural spread of inflammation causes lymphedema and thickening of the intestinal wall and mesentery. Mesenteric fat typically extends to cover the serous surface of the intestine. Mesenteric lymph nodes often enlarge. Extensive inflammation causes hypertrophy of the muscularis mucosae, fibrosis and stricture formation that can lead to intestinal obstruction. Abscesses are frequent and fistulas often penetrate nearby structures, including other intestinal loops, the bladder or the psoas muscle. Fistulas can also extend to the skin of the anterior wall of the abdomen or flanks. Regardless of intraabdominal disease activity, perianal fistulas and abscesses appear in 25–33% of cases; these complications often represent the most troublesome aspect of Crohn's disease. Non-caseating granulomas can form in the lymph nodes, peritoneum, liver and all layers of the intestinal wall. Although pathognomonic when present, granulomas are not observed in approximately half of patients with Crohn's disease. The presence of granulomas does not appear to be related to the clinical course. and diseased areas of the intestine are well delimited from the adjacent normal intestine (so-called sparing areas):
• About 30% of cases of Crohn's disease involve the ileum alone (ileitis).
• Approximately 40% involve the ileum and colon (ileocolitis), with a predilection for the right side of the colon.
• About 30% involve only the colon (granulomatous colitis), most of which, unlike ulcerative colitis, spare the rectum.
The calprotectin value is immediately very high (around 600 mcg\g), therefore pathognomonic of an ongoing chronic inflammatory disease.
Calprotectin is a protein belonging to the S100 family and is present in large quantities in neutrophilic granulocytes, where it represents 5% of the total proteins and 60% of the cytoplasmic proteins. In smaller quantities, calprotectin has also been found in activated monocytes and macrophages. The structure of calprotectin consists of one light polypeptide chain and two heavy polypeptide chains and has a total molecular weight of 36.5 kDa. It is a protein with bacteriostatic and mycostatic activity comparable to that of antibiotics: for this reason the abundance of calprotectin in neutrophilic granulocytes and its antimicrobial activity suggest an important role in the defensive functions of the organism. The presence of calprotectin has been found in various human biological materials: in serum, saliva, cerebrospinal fluid and urine. However, it is the dosage of calprotectin present in the feces that offers the greatest advantages in evaluating the degree of inflammation of the intestine: calprotectin is in fact an extremely stable protein in the feces, where it remains unchanged even for more than 7 days. In the presence of processes inflammatory, calprotectin is released following the granulation of neutrophilic granulocytes. In the case of inflammation of the intestine, calprotectin can be detected in the feces. The fecal dosage is the only one that can provide direct indications on the localization of the inflammation, while the dosage in serum or plasma highlights a state of inflammation that can be localized anywhere. The increased concentration of calprotectin in the feces is a direct consequence of neutrophil granulation following mucosal damage. The measurement of calprotectin in feces offers significant advantages in the evaluation of intestinal inflammation.
The patient performs ileocolonoscopy which confirms the thickening of the mucosa of the terminal ileum with the characteristic 'cobblestone' appearance, caused by the lifting of the healthy mucosa by the impressive change that the submucosal layer undergoes (lymphedema), the so-called transmural inflammation ; the stenotic attitude of the viscera with marked reduction of the central lumen is also evident; the biopsy shows the presence of granulocytic infiltration, and lymphocytes, plasma cells, macrophages and eosinophils, effectively confirming the diagnosis of Crohn's disease in the productive phase.
The patient therefore decides to follow the immunosuppressive therapy course at the gastroenterology department of the Sant'Orsola hospital in Bologna.