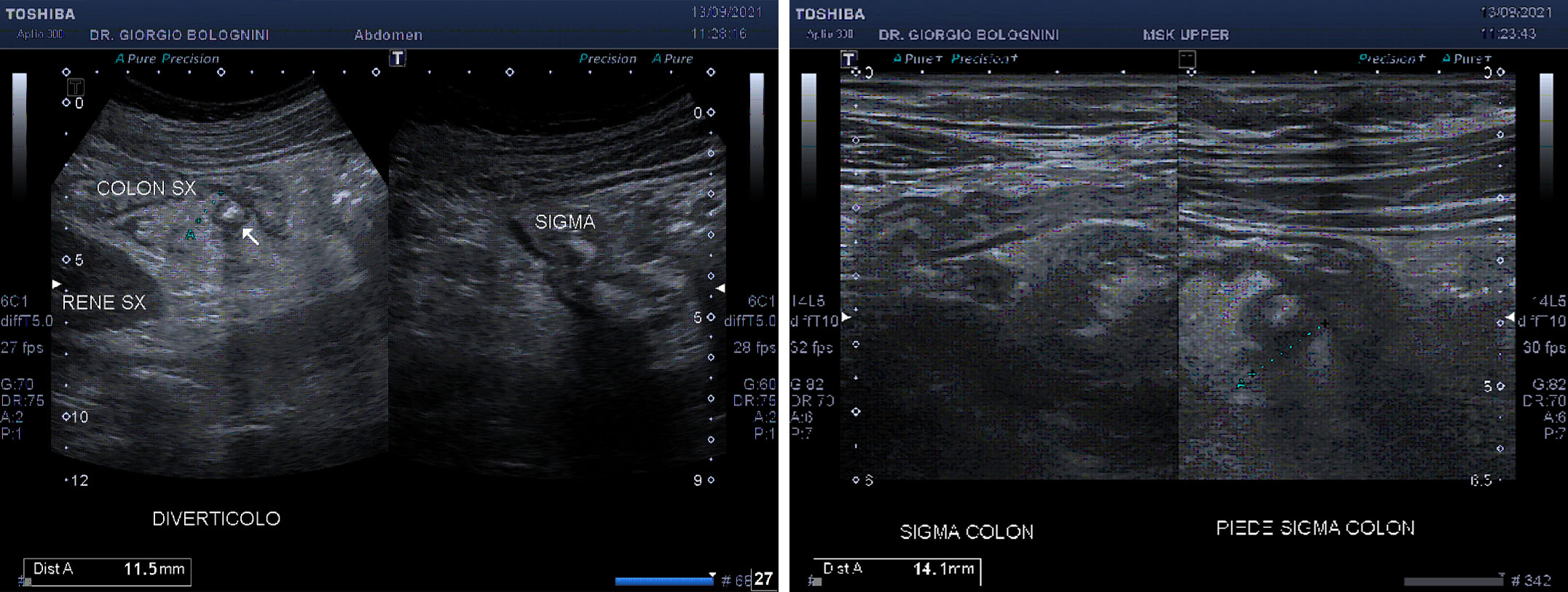
A 71-year-old woman, with a familiarity with pancreatic cancer (deceased mother), hypertension and hypothyroidism, with previous ileo-colonoscopy that showed a context of non-pathological shrinkage of the right colic flexure, came to the clinic due to pain in the right colic flexure associated with mild hyperpyrexia (37.8 C); the abdominal ultrasound study conducted urgently (therefore without adequate dietary and intestinal preparation) both with convex and linear probe, detected the presence of diverticular eversion with a dense content of the anterior wall of the sigmoid colon of about 14x12mm, with minimal signs of perivisceral exudation and hyperechoic thickening of the mesentery.
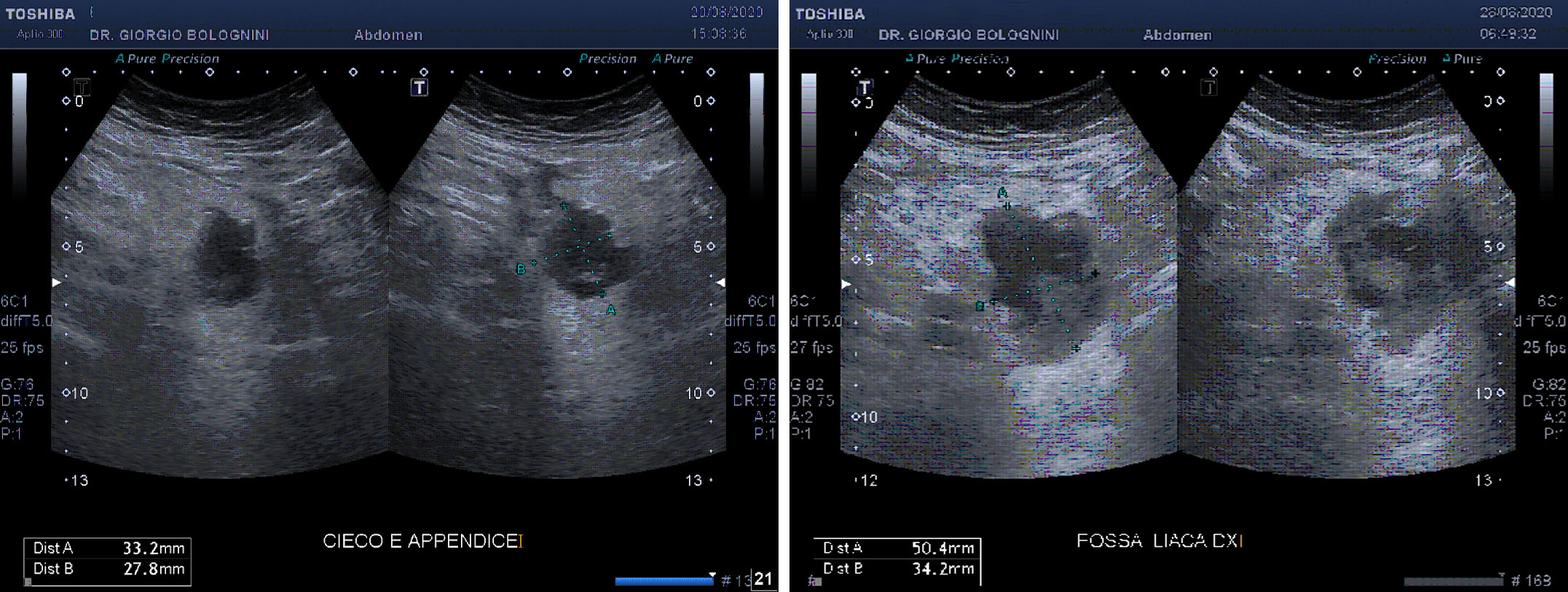
The patient began antibiotic therapy with ceftriaxone 1gr once daily and carried out blood tests showing increased rates of inflammation and leukocytosis (GB 13,400, N 82%, L 6.8%, haemoglobin 11, ESR 65, PCR 3.28). After four days of antibiotic therapy due to even more acute pain and a marked increase in body temperature (39 C), the patient returned to my ultrasound clinic for an urgent examination, with evidence of pseudo-abscess formation attached to the anterior wall of the proximal sigma of about 54x33mm with complex echo structure, hypoechoic with hyperechoic internal echoes (probable gaseous artefacts) and hyperechoic central core. The presence of internal vascular signs cannot be demonstrated with the device supplied. Presence of peri-abscess lymph node posterior to the sigma of about 12mm and important hyperechogenicity of the mesentery for acute inflammation (peritonism).
The patient was sent to Cisanello hospital surgery (the Professor Luca Morelli team at the SD General Surgery 1 Univ Osp Cisanello Pisa, Director Prof. Giulio Di Candio) with a presumed diagnosis of perforated diverticulum in peritonitis: the sigma resection operation was followed urgently as a result of the CT confirmation of visceral perforation.