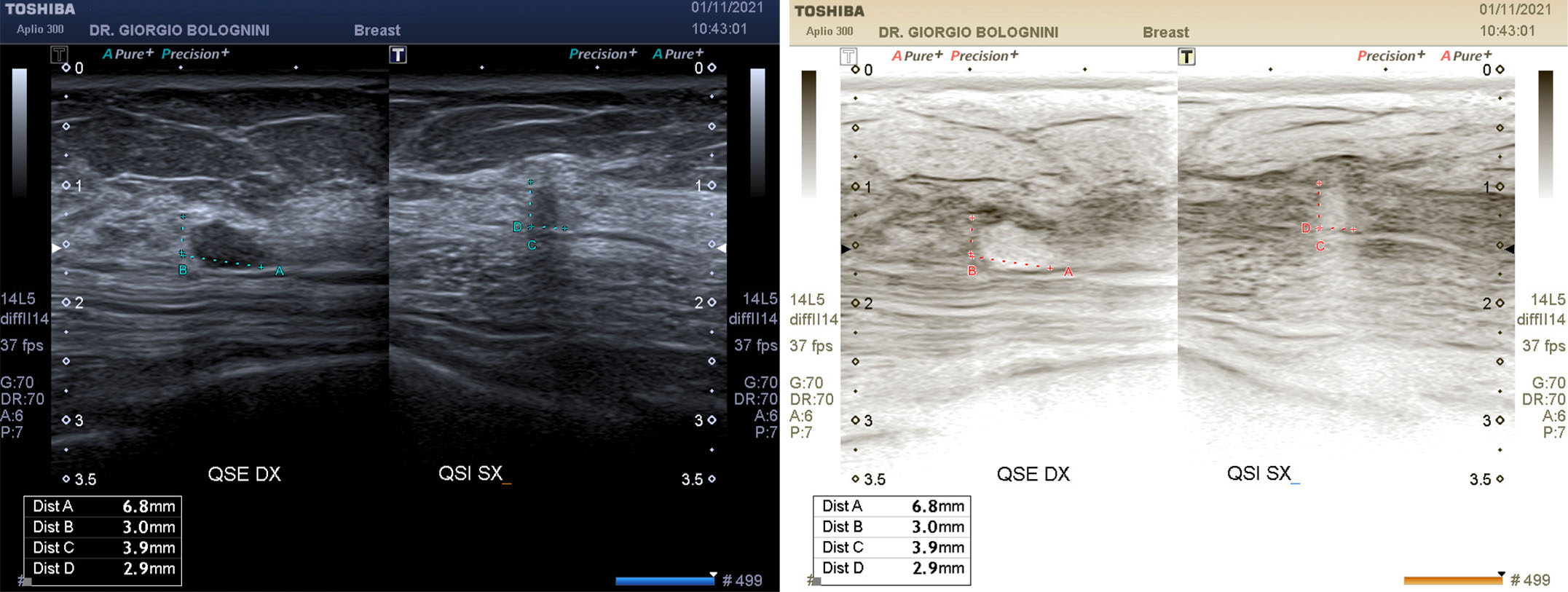
69-year-old woman, undergoing annual ultrasound control due to persistently hyperechoic glandular breasts, which can be easily explored with mammography; ex smoker, three pregnancies with natural childbirth, hypertensive, dyslipidemic, with a mild respiratory insufficiency of a predominantly restrictive type. In her breast history she does not report family members operated on for breast cancer; carrier of B2 mammary fibroadenoma at the level of the right QSI of about 7x3mm, dimensionally stable morpho for years. At the last ultrasound check, I identify an area of blurred acoustic impedance on the deep planes of the left QSI of about 3.5x4.1mm, with a nodular shape, not present in the previous checks, with a small simple adjacent cyst; the 'taller than wide' appearance, and the tenuous posterior shadow cone generated by the small nodule raise the suspicion of U3 formation.
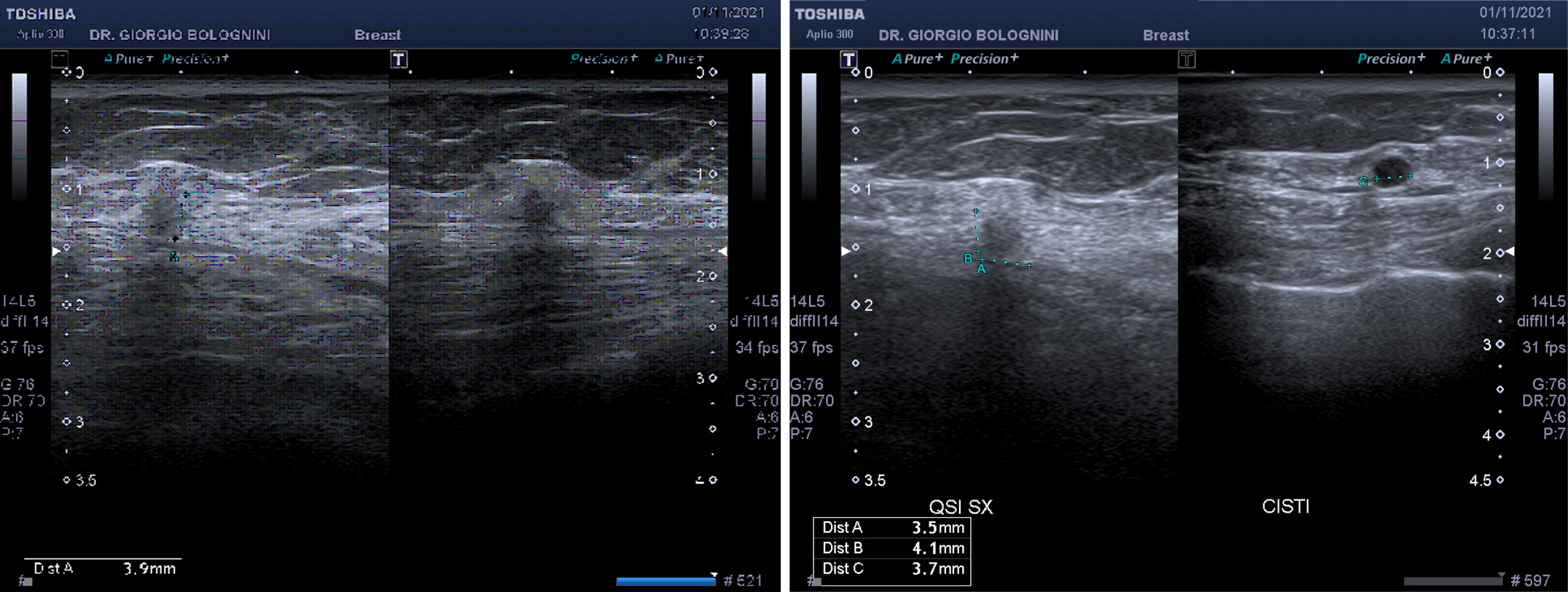
The very small size and the scarce surrounding parenchymal distortion do not help in the possible diagnosis of malignancy; for which I request an immediate new mammography check-up (the last was about 10 months earlier). However, the ultrasound comparison with the right QSI fibroadenoma does not leave much hope on the nature of the nodule; the main difference, in addition to the oval shape of the AF versus the rounded shape of the nodule, is again in the acoustic impedance generated on the underlying floors. The iconographic post processing carried out at a later time with a negative image clearly shows this phenomenon on the deep planes.
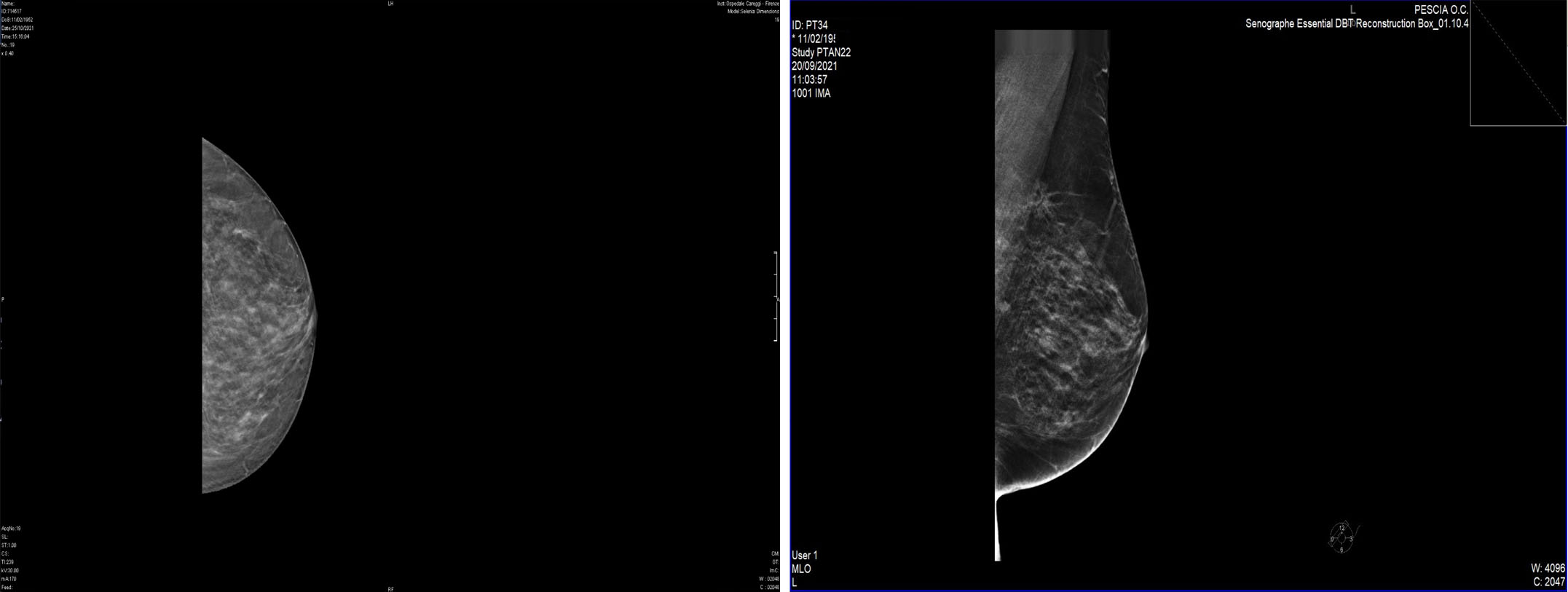
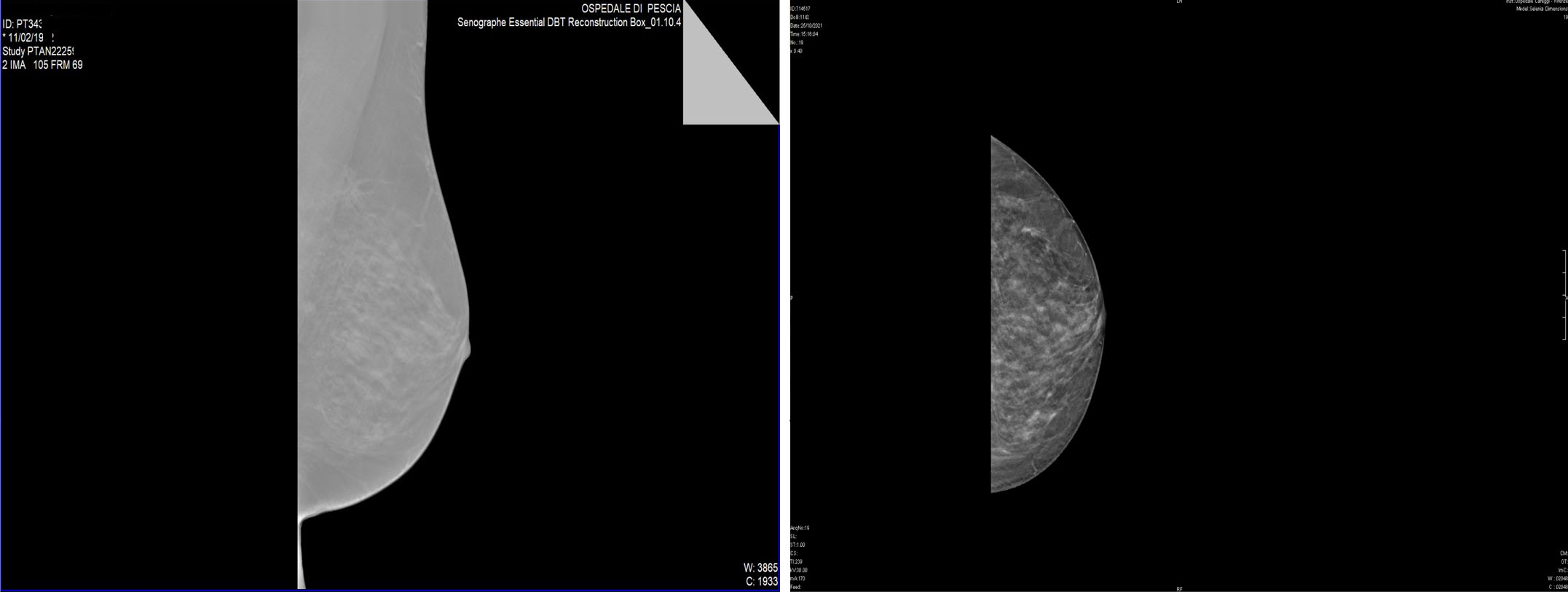
Mammography confirms the presence of a small area of parenchymal distortion on the deep planes of the left QSI, with a polylobed shape, not present in the previous control, without R3-type microcalcifications.
For further confirmation, the patient is invited to perform a breast MRI, which, however, due to the presence of metal wires from previous maxillofacial surgery, must be replaced with a CESM (contrasted enhanced spectral mammography) mammography at the Careggi Hospital; the examination identifies two areas of impregnation type irregular adjacent mass and with a maximum size of 16 and 12mm with a total extension of 31mm, referable to the index lesion; it is not possible to evaluate the relationship with the pectoral muscle behind it because the lesions are only partially included in the field of view of the method.
The patient is then subjected to a tru-cut biopsy with the following histological result: invasive carcinoma of the breast of the infiltrating lobular type: immunohistochemistry: REC ER 95%, REC PgR 15%, KI67 8%, HER2 \ NEU negative. The patient is then subjected to total left nipple-sparing mastectomy with prosthesis placement and sentinel lymph node biopsy with OSNA technique (negative result, therefore T1c N0 M0) at Santa Chiara Hospital in Pisa, by professor Manuela Roncella, director of the Clinical Center of Senology - AOU Pisana. Subsequent hormone therapy with 2.5mg letrozole follows, given the good expression of estrogen receptors. The pathological anatomy report was as follows: invasive lobular carcinoma classic variant G2 of 18mm + classic and florid variant carcinoma. The patient is undergoing a six-monthly ultrasound follow-up.